Amblyopia can be defined as the deficient development of brain vision during the first decade of human life, and is the topic of some excellent recent reviews.1–3 It remains a common cause of vision impairment in developed countries despite the fact that it is completely preventable and treatable. In some small-scale regional efforts in developed countries, deliberate screening combined with consistent therapy has produced dramatic reductions in amblyopia prevalence and severity.4–6
World Health Organization Screening Criteria
Amblyopia can be defined as the deficient development of brain vision during the first decade of human life, and is the topic of some excellent recent reviews.1–3 It remains a common cause of vision impairment in developed countries despite the fact that it is completely preventable and treatable. In some small-scale regional efforts in developed countries, deliberate screening combined with consistent therapy has produced dramatic reductions in amblyopia prevalence and severity.4–6
World Health Organization Screening Criteria
Ten criteria have been developed by the World Health Organization (WHO) by which community health screenings can be evaluated for potential benefits and affordability:7 is it an important health problem?; accepted treatment for recognised disease; facilities for diagnosis and treatment; suitable latent and symptomatic stage; suitable test or examination; test acceptable to population; natural history of condition understood; agreedon policy on whom to treat; cost of finding an economic and overall health balance; and case finding should be continuous. These criteria have been applied to many processes, including vision screening for amblyopia. There have been several prominent publications and programmes that have opposed or bypassed vision screening for amblyopia. In part, this article will focus on how several major detractors of paediatric vision screening are no longer consistent with WHO screening guidelines.
Evidence-based Medicine
The concept of evidence-based medicine requires various types of research to be hierarchically ranked in order of their pertinence and reliability, from which current knowledge concerning health interventions can be evaluated, e.g. a well-controlled, randomised clinical trial would receive higher priority than case studies or population observations. Although the US Public Health Service (USPHS) has come out with a moderately strong backing for amblyopia vision screening,8 the renowned Cochrane Collaboration has not yet given vision screening a favourable endorsement.9 This echoes a controversial report of major importance by Snowdon in the UK, which failed to find studies of sufficiently high hierarchy for paediatric vision screening and therefore recommended disbanding such efforts in the UK.10
Is Amblyopia an Important Health Concern?
Rahi et al. reviewed the outcome in a cohort of 8,432 people of whom 429 had amblyopia to determine whether these amblyopic people functioned differently from their binocular counterparts.11 With respect to “educational outcomes, behavioural difficulties or social maladjustment, participation in social activities, unintended injuries (school, workplace or road traffic accidents as driver), general or mental health and mortality, paid employment, or occupation-based social class trajectories”, there was not a substantial difference. This conclusion cast doubts on the value of vision screening for amblyopia. Nilsson similarly questions the merits of pre-school acuity screening based on presumed better utility of amblyopic adults12 than that estimated by Beauchamp.13
Disabled people are frequently inspiring. Special Olympic athletes, injured veteran wheelchair athletes and blind mountain climbers garner cheers from audiences worldwide. A disabled person with a good attitude, or with a need to survive, has a great ability to adapt, even to fail in spite of the disability. As an internist my father was once carrying out a physical examination on an ex-Marine back from the war and could not view one retina. The military excludes monocular recruits from battle. When queried, the Marine smiled and admitted he had lost his eye and had an artificial eye long before enlisting. During each of his military physical exams, he did what many paediatric patients do: peek on their acuity tests. Instead of having his untested eye patched as the American Academy of Pediatrics (AAP) recommends,14 this Marine covered his blind ‘eye’ with the right hand for the first eye, and when the tester glanced at his acuity chart, the soldier switched and covered the same prosthesis with his left hand. Instead of admitting his disability and being limited by it, he was appropriately proud of having served his country.
Despite residual amblyopia from late-detected bilateral hyperopic amblyopia, the risk of loss of the sound eye remains higher for amblyopic patients.15 There is substantial cost to society from residual vision loss due to amblyopia.16 Ophthalmologists do their best to help adult patients with residual vision loss due to amblyopia, but it is not the same. Safety glasses are strongly encouraged and amblyopic patients are often denied contact lenses or elective refractive surgery by conservative ophthalmologists. Amblyopic patients are considered ‘one-eyed’ with respect to risk–benefit discussions of cataract surgery or retinal surgery. Therefore, the concern is not whether amblyopic patients can adapt and function; vision screening addresses the matter of whether society is ready to allow children to develop or retain the residual vision impairment. The wheelchair athlete does not want her child to have a leg taken off. The blind climber does not ever want to let his child go blind. Similarly, public health policy makers should not deny amblyopia screening and treatment because some adult amblyopic patients can adapt to their disability.
Accepted Treatment for Recognised Disease
The previous lack of large-scale randomised studies for amblyopia have now been addressed by the National Institutes of Health (NIH)- supported Pediatric Eye Disease Investigator Group (PEDIG) in a series of evolving, related Amblyopia Treatment Studies (ATS). It is now clear that amblyopia can indeed be treated,17 that refractive correction is extremely important18–20 and that patching works when the benefit of spectacles has plateaued.21
Facilities for Diagnosis and Treatment
In developed countries the diagnosis of amblyopia, or conditions leading to it, are easily performed by eye doctors with experience in dealing with small children. A ‘confirmatory examination’ differs from a low-risk general population comprehensive exam because the patient is a child referred for vision screening and therefore is at higher risk. The exam follows a directed history and determines age-appropriate acuity, with monocularity assured by patching the non-tested eye. Pupils and peripheral fields are tested in addition to general observations of the patient, neuro-status, head, orbits and ocular adnexa and ocular media clarity. The refraction includes determination of accommodative status, ideally with dynamic retinoscopy or office photoscreening, and then cycloplegic refraction. Finally, the retina and optic nerve are examined.
Treatment is primarily office- and home-based with spectacles and/or contact lenses prescribed and fitted. Patching and/or atropine penalisation are carried out at home. Outpatient surgery may be required for ocular media opacity, eyelid obscuration of vision or strabismus. However, in developing countries facilities are scarce and intermittent screening, remote exams and spectacle delivery are usually possible on a charitable basis only.22 Crude occlusion patches can be constructed from adhesive tape. Patients reluctant to comply with occlusion may be offered sutured occluder treatment to afford four weeks (400 hours) of full-time patching and an expected 3 logMAR lines of acuity gain.23 There is strong evidence that the main benefit from patching occurs within 170 hours in a child four years of age and within 236 hours in a child six years of age.24,25 Indeed, children with a severe risk factor for congenital cataract who have good intraocular lens and initial patch therapy may even retain26 good acuity with ‘early’ discontinuation of intense patch therapy.27
Suitable Latent and Symptomatic Stage
There is conclusive evidence for a latent period in human amblyopia, although it does not correlate exactly to animal evidence from Hubel and Wiesel28 and von Norden.29 Early intense intervention with unilateral congenital cataract before six weeks to four months of age results in better acuity.30 Amblyopic children detected by photoscreening before two years of age had 1 logMAR line better treatment acuity than those detected between three and four years of age.31 In the PEDIG ATS Number 1, longterm follow-up in premier paediatric eye practices showed better eventual acuities in those starting at less than five years of age (20/25) versus those starting at five or six years of age (20/32).32 PEDIG also found worse responses to amblyopia treatment in older teens than in pre-teens.33 Therefore, there is an obvious latent period and advantage with respect to outcome acuity with early detection.
Amblyopia in children may not be symptomatic. Posterior congenital cataracts (rare) and anisometropia (common) are extremely occult. Constant strabismus is usually observed early by parents34 and this has excellent predictive value in amblyopia screening.35 Risk factors for most cases of amblyopia include high refractive error, constant strabismus and ocular media opacity. Although many of these may not be directly observable in pre-literate children, objective screening – i.e. the Brückner Test – photoscreening and remote autorefraction35 can detect all of these factors in young children and infants.
Suitable Test or Examination
Amblyopia is the sensory loss of potentially learned brain vision, primarily in the central visual field, and therefore is represented by diminished bestcorrected visual acuity. For this reason, paediatrician and community screening of monocular acuity has been the mainstay of amblyopia screening. Indeed, acuity screening can be a suitable tool for detection. Objective tests are designed to reveal amblyopia risk factors from passive children. Photoscreening emits flashes of light relatively coaxial to the camera lens, which allows an analysis of reflected crescents of light reflected from defocused or misaligned eyes36,37 and is related to dynamic retinoscopy.38 Remote autorefraction determines refractive error by wavefront analysis.39 Both photoscreening and remote autorefraction can detect high levels of refractive error, which are amblyopia risk factors.
An eye examination can also detect amblyopia and risk factors for amblyopia. Paediatric ophthalmologists usually perform complete examinations on infants referred with tear duct obstruction40 and therefore detect and treat amblyopia in about 5–10% of cases. When balancing the cost and benefit of overall paediatric care, the AAP does not recommend a complete eye examination unless the child is symptomatic or fails a series of age-appropriate vision screenings.14 On the other hand, organised optometry and optical dispensing industries have proposed and implemented community programmes designed to use widespread paediatric complete examinations in part to detect amblyopia and several other vision and learning-related conditions. A programme called ‘InfantSEE’, sponsored by Johnson & Johnson, is designed to encourage optometrists who visit their Florida resort centre to perform checks on children six months of age.41 Another programme is called ‘Check Yearly—See Clearly’, which espouses annual exams for all children.42 The American Optometric Association (AOA) has promoted ‘mandated prenursery eye examinations’, which are now adopted as law in Kentucky,43 Missouri and Illinois. The AOA recommends that children have a complete eye examination every two years.44 It is worth remembering that these examinations are performed on low-risk populations and are therefore ‘comprehensive eye exams’ and not confirmatory exams. So, screenings and exams can detect amblyopia; which are suitable? This requires evaluation of validity. Matters of cost-effectiveness will be covered in a subsequent WHO guideline section.
If a group of young children after careful confirmatory examinations were sorted into a group at high risk of amblyopia or with amblyopia versus those without amblyopia, you would have ‘true’ and ‘false’ groups. Screening sorts the entire group into high risk versus low risk. A measure of how well the screening finds all of the true patients is sensitivity. Another important validation statistic is specificity, which determines how well the screening identifies the true or false. The proportion of those who screen positive who actually are true are called ‘predictive value’. In a ‘real-world’ community screening, predictive value can be determined by performing confirmatory exams on just the small percentage referred, whereas determining sensitivity and specificity requires performing confirmatory exams on all of the children. The number of studies needed to accurately achieve this is small because such studies are expensive.45,46 The NIH-supported Vision in Pre-schoolers Studies (VIPS) used a disease-enhanced population; therefore, it is a variation on an ideal validation study.47,48
It is extremely important that validation studies use identical standards or else the paediatric community will be ‘comparing apples with oranges’. The American Association for Pediatric Ophthalmology and Strabismus (AAPOS) proposed and published such a list of conditions that may be found in a confirmatory exam to place a pre-school child at sufficiently high risk of developing amblyopia.26 VIPS later developed more complex groups of amblyopia risk factors,47 but unfortunately has not published its results using the AAPOS guidelines.49
A graphic representation of how sensitivity and specificity change for a given screening – by varying the referral criteria – is called the receiver–operator characteristic (ROC) curve.50 Interpretations from most screenings can be divided into ‘refer’, ‘pass’, ‘unable to test’ or ‘inconclusive’. Screenings that have a high proportion of inconclusive/unable to test are of less value than those that provide a definitive answer for each child screened, unless it is simple for technicians and parents to repeat the screening. The Alaska Blind Child Discovery (ABCD) project has defined a new set of validation statistics that incorporate inconclusive/unable to test results into the denominator, therefore favouring definite interpretations, and are particularly applicable for rural and remote screenings.51,52
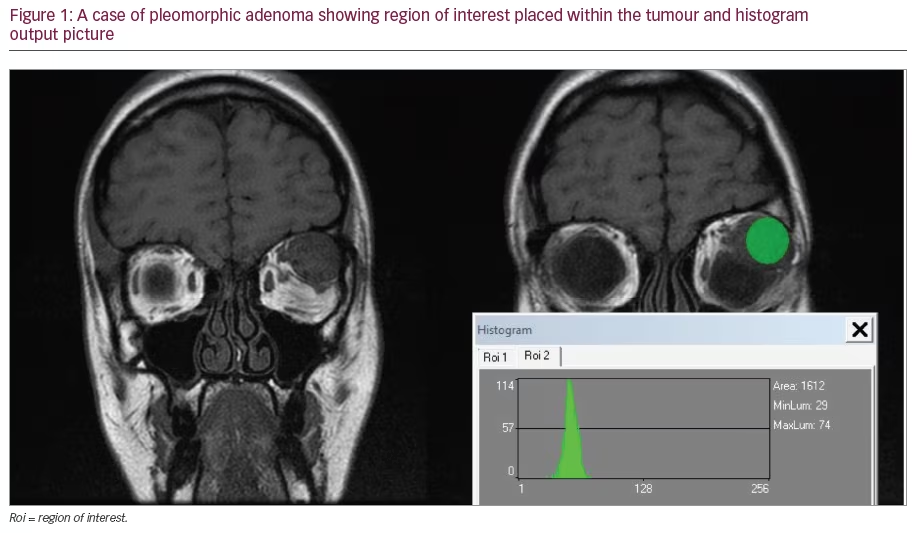
‘Conventional vision screening’ is acuity testing with various methods to assure monocularity and is, relatively speaking, the ‘new kid on the block’. A number of prominent paediatric ophthalmologists assume that acuity screening is inexpensive, easy and reliable, and therefore are sceptical about objective screening that involves potentially expensive equipment. Few academic paediatric ophthalmologists have spent time ‘in the trenches’ performing community mass paediatric vision screening themselves. Careful development, validation and improvement of vision screening is difficult.46,53 It is much easier to scientifically demonstrate the imperfection of a new method than it is to innovate and develop. To date, the most extensively used technology has been Howard Freedman’s Polaroid-based, sequential, orthogonal, off-axis MTI photoscreener (see Figure 1).54 It is much easier for paediatric ophthalmologists to apply vision screening technology to their own enhanced-prevalence practices and determine that vision screening is not perfectly valid55–58 or difficult to interpret.56 Some noble developers of objective screening technology, facing a hostile business and legal climate, have also suffered relative academic humiliation, discouraging some from advancing their prototypes to better versions.54,59–61 There is clinical evidence that emerging objective technology can outperform acuity screening in terms of validity, speed, testability, screener skills and acceptability.62–65 With time, experience and encouragement, vision screening with consistent, monocularity-assured acuity testing can be performed in co-operative pre-schoolers.5 In a practical sense, mass acuity screening of children is much more feasible after nursery age, and is not feasible children with language or developmental disabilities.66,67 Therefore, it is not a question of whether objective tests or acuity tests are better: they should be used in age-related sequence during the years of amblyopia susceptibility.
A profound mistake in amblyopia screening is to focus too much on sensitivity rather than on the predictive value and its inversely related specificity. Manufacturers and paediatricians favour the most sensitive test because they are afraid of missing any low-vision children in that single test. Remember that the AAP recommends a series of tests rather than a single test. Parents and busy paediatric ophthalmologists favour a test with high specificity manifest in high positive predictive value. When 10 new children are referred from a screening, it is encouraging if at least seven have real amblyopia risk. When polled, primary care doctors wanted a vision screen with predictive value over 90%;68 few programmes have achieved this low false-positive rate.51 The ROC curve shows that when sensitivity goes up, specificity will go down, and vice versa.
The three-phase VIPS were designed under the assumption that a single pre-school screening or exam was sensitive enough to detect all cases of amblyopia. Consequently, commercially available vision-screening technology was compared with referral criteria either pre-determined (MTI and iScreen) or in-study calibrated with a relatively low specificity to yieldcompared sensitivity.47 The first phase of VIPS was performed mainly by expert paediatric optometrists, with 11 screenings, including patched acuity, performed in pre-school head-start children. Due to the potential photoreceptor wash-out of the camera flash, the photoscreeners were not randomised in order, but rather performed at number 10 and 11 (last) of all tests. Two objective tests had high sensitivity for VIPS criteria: the Welch Allyn Suresight (remote autorefractor) and the Nikon Retinomax, which touches the child’s face. However, the photoscreeners (MTI with voice interpretation), iScreen and the precursor to PlusOptix failed to make the sensitivity threshold to continue into phase two of VIPS. VIPS did not include the other photoscreeners (EyeDx or Vision Research). VIPS phase one showed that the paediatric optometry exam outperformed all available screening technology with respect to sensitivity; however, paediatric optometry dynamic retinoscopy was also quite sensitive. Initially, VIPS was to have had three phases, starting with expert paediatric screening professionals and then moving through skilled nurses (phase two) and finally to lay screeners (phase three). Unfortunately, the validity of the technology surviving VIPS phase one faltered in phase two, with referral criteria for patched Lea acuity moved to five feet from 10 feet and referral criteria Welch Allyn Suresight further calibrated by study, with the result that VIPS three was never funded. One false conclusion made from phase one of VIPS was that comprehensive community optometry exams were better than any available screening technology; this has been used to promote mandated pre-nursery exams. Community comprehensive non-cycloplegic eye exams are not the confirmatory paediatric subspecialty exams of VIPS.
Are the available screening tests suitable for screening all pre-schoolers regardless of age? Do they work in infants, toddlers and nursery-age children? The testability rates of the VIPS-favoured Nikon Retinomax falls off under four years of age.64 The Welch Allyn Suresight can have reasonable testability down to less than three years of age, but has reduced predictive value.69 Remote objective tests such as Brückner or MTI photoscreening have similarly high testability and predictive value down to one year of age.35 From a practical standpoint, in prominent paediatric practices photoscreening outperforms acuity testing in pre-schoolers.62 A less dramatic advantage of photoscreening over acuity testing has been observed in school-based screening of younger students.66 Acuity testing with monocularity requires a high level of expertise of screeners, but can be a suitable screening tool for children as young as four years of age.5 The prevalence of amblyopia varies between communities, but it is probably between 2 and 4%.45 Strabismus occurs in about 2.5% of children, with the frequency increasing after three years of age. An overlapping 2% have amblyopia, of whom 80% have abnormal refractive error that can be detected by objective screening. Experienced, widespread charitable photoscreening has a referral rate of 5–6% with a predictive value of 75–85%, indicating that Alaska has at least a 5% AAPOS guideline condition prevalence, whereas Tennessee has about 3.5%. We hope the Multi-Ethnic Pediatric Eye Disease Study (MEPEDS) group will publish the prevalence of AAPOS-guideline gold standard conditions.26 If the prevalence of conditions such as strabismus and amblyopia in a defined population cohort are known, reliable estimations of validity to future technology will be much easier and cheaper than with the VIPS study.70
If paediatric vision-screening methods are applied to children who do not have obvious strabismus, developmental delay or syndromes or strong family histories, no-one knows whether or not they have amblyopia until a confirmatory exam is performed. Amblyopia risk factors are known to evolve in some children. As long as a series of age-appropriate screenings is applied, initial screening with high predictive value will be best, followed by more sensitive tests at later ages. Two long-standing, state-wide specific photoscreening studies emphasised the specificity of age-related tests instead of setting referral criteria that were too sensitive; neither has had adverse eventual sequelae from presumed false-negative results.71 Other objective programmes can achieve similar success.72 For these reasons, specific photoscreening during pre-school and nursery entry followed by sensitive, patched, surround/crowded logMAR acuity is favoured by the ABCD project.52
Is the Test Acceptable to the Population?
This depends on cost, availability, scheduling and whether or not it is child-friendly. Vision screening is not painful unless the occlusive acuity no-peeking patch has a strong adhesive. Vision screening does not require removal of clothing and is non-invasive. The flash of some photoscreeners will make young children upset, but not as much as the close remote autorefractors, i.e. Nikon Retinomax. On the other hand, treatment requires glasses that many people consider socially unacceptable or not durable. Neither patching nor atropine penalisation is easy, although the former is less preferred for many families.73 School attendance is more difficult with atropine therapy even though compliance may be better. Surgery scares many families and may not be affordable. The current screening methods are well accepted by most families in developed and developing countries. In general, courses of amblyopia therapy are fairly well accepted. Better data on the level of intensity of therapy and the duration of therapy for a given patient would greatly enhance this. Parents and paediatricians would like to know when the amblyopia therapy is complete so that their child will not lose vision when they stop optical and preference therapy.
Natural History of Condition Understood Studies of Non-compliance
Of the WHO screening criteria, this is the least defined area with respect to paediatric amblyopia screening. This is because there have not been many long-term, large-scale population studies that carried out confirmatory exams on several thousand infants, only to monitor them annually with those having significant amblyopia risk factors remaining untreated. The UK Avon Longitudinal Study of Parents and Children (ALSPAC) received institutional review board (IRB) approval to deliver extra versus additional levels of amblyopia screening and randomised treatment as both arms of the study provided more care than leaving children outside the study; ALSPAC found that the screened children had high levels of hyperopia. Crosssectional studies demonstrate that the proportion of children with strabismus, specifically accommodative esotropia and associated amblyopia, increases with age.45 Toddlers referred by photoscreening and receiving treatment had better acuities than children detected one or two years later.31 Studies on non-compliant amblyopic cases suggest that either they do not achieve the expected recovery of acuity23 or they regress.74
Agreed-on Policy on Whom to Treat
Mandated Exams versus Defined Amblyopia and Risk
The PEDIG studies suggest that there is a relatively wide window for starting optical and patching therapy in literate children four to seven years of age. However, waiting more than one year with a known amblyopic child, particularly one with more severe amblyopia, is not consistent with PEDIG findings. There has been concern that early correction of hyperopia may interfere with emetropisation; however, the ALSPAC study would argue against this.6 Little has been published in terms of ongoing care compared with the timing and initial dose of amblyopia therapy.75 It is much less clear at what age therapy – including optical – can cease.
Lempert noted anatomical differences in the eyes and optic nerves of children with conditions others may pass off as purely anisometropic amblyopia.76–79 Other children have decreased acuity combined with partial media opacity, nystagmus, developmental delays, etc., and are rarely included in randomised studies such as PEDIG ATS. Large-scale, prospective amblyopia studies have far more reliable data on starting amblyopia therapy than appropriate adjustments or dosages during ongoing therapy. Any prospective study on amblyopia that requires acuity for entry limits our data on the potential merits of pre-literate, amblyopia treatment or prevention in children referred by objective screening.31 Therefore, additional constitutional and ocular conditions may modify the ideal outcome of amblyopia therapy (glasses, contact lenses, patching and/or atropine).
Paediatric ophthalmologists agree on the merits of giving a robust initial effort and persisting for as long as benefits are documented. One of the main factors in amblyopia success is therapy compliance because, apart from patient frustration with blurring or occluding the sound eye, some dislike their spectacles or contact lenses. Achieving compliance is usually a matter of discipline in the home. Some paediatric ophthalmologists consider therapy non-compliance ‘child abuse’ and therefore invoke assistance with state protective services. Others seek optical,80 chemical81 and surgical methods23 to improve amblyopia therapy compliance. Even for a child with socioeconomic, systemic and ocular co-morbidities, almost all paediatric ophthalmologists will offer amblyopia therapy to those younger than eight years of age, and recent PEDIG studies suggest that efforts should be addressed to children even older than that.33
The PEDIG ATS have proved the equivalence of shorter-dose patching and atropine for moderate and severe cases of strabismic, anisometropic and mixed amblyopia. In addition to showing benefit of the lesser treatment, ATS showed no adverse effects of the randomised arm, higher dose patching or atropine. As such, several initial doses of patching are considered acceptable. Atropine daily or on weekends is useful for children on sufficiently hyperopic prescriptions.82
Cost of Finding an Economic and Overall Health Balance
For screening to be affordable, there must be some benefit in terms of either productivity gained or costs avoided. Screening costs more than no screening during the latent and treatment phase. With respect to amblyopia, a child who is screened and successfully treated and has two functioning eyes rather than just one may qualify for several jobs, e.g. law enforcement, armed services or transportation. The direct employability with respect to appearance will be enhanced by stable binocularity and the ability to wear contact lenses instead of having manifest strabismus or conjunctival evidence of multiple strabismus re-operations. The bilateral patient is less likely to lose the better eye following an accident.15 There is substantial disability if one eye is injured or lost due to asymmetric disease: loss of one eye is considered 24% of a person whereas loss of both is considered the loss of 75%, according to US disability determination guidelines.83
Objective screening, despite the expense of a photographic device, may have more cost benefit than sensory testing.84 Photoscreening takes far less time than careful acuity screening,63,66 and ‘time is money’ in terms of staff salaries and programme interruptions. A cost–benefit study sponsored by the Vision Council of America (VCA) (optical industry group) found that comprehensive exams were more cost-effective than liver transplants.85 Further analysis of that study revealed that vision screening was far more cost-effective, measured by quality-adjusted life-years (QALY), rather than comprehensive exams.86 When vision screening costs are combined with resultant costs to provide appropriate eye care over the first decade of life, AAP vision screening enhanced by early photoscreening outperforms the use of comprehensive single or serial eye exams.87 The quality of follow-up exams after vision screen referral varies, and there can an additional cost of overprescription of spectacles in many cases of comprehensive community examinations of children’s eyes.88
Case Finding Should Be a Continuous Process
Some patients followed-up with annual cycloplegic examinations and treated for amblyopia will have evolving degrees of astigmatism, hyperopia and anisometropia, suggesting that amblyopia risk factors may be evolving in the unscreened population as well. Therefore, a single effort, no matter how sensitive, will not detect and treat all cases. On a practical basis, comprehensive eye exams of low-risk, hungry, agitated pre-nursery children by a community doctor will have far less sensitivity than careful research confirmatory exams carried out by paediatric optometrists.47 The AAP guidelines recommend a series of age-appropriate objective and sensory tests, starting with newborns, incorporating history and parent-detected signs and symptoms.14 Recent research31,89 strongly suggests that previously indicated photoscreening90 be incorporated into new AAP guidelines and appropriately reimbursed, ideally between the age of 12 and 24 months, again between 30 and 48 months and, if available, as a more valid alternative to acuity testing in nursery-entry screening. Sensitive acuity testing with monocularity assured by patching should follow66 until children mature beyond their first (amblyopia-susceptible) decade.
Conclusion
Paediatric vision screening for amblyopia, particularly using AAP guidelines, in concert with early objective screening appears to comply with WHO guidelines for health screening. A practical implementation of such screening in the US is primarily impeded by the lack of uniform reimbursement for early objective screening, combined with lazy utilisation of patched, crowded/surround logMAR acuity screening. The majority of strabismic amblyopic patients have moderately large-angle esotropia and are detected well by parents and attentive paediatricians. Eighty per cent of amblyopic patients have a significant refractive error that can be efficiently detected early by photoscreening and remote autorefraction. If the leaders in the US support and reimburse objective screening, industry will respond with technology that is far more efficient, portable and affordable than current models. As with other healthcare systems, yesterday’s state-of-theart technology from developed countries soon becomes effective when donated, or discounted, for worldwide use. The ‘Magic Number’, current procedural terminology (CPT) code 99174, if well reimbursed and utilised, promises to have a profound impact on amblyopia vision impairment worldwide by promoting research and development in this field.