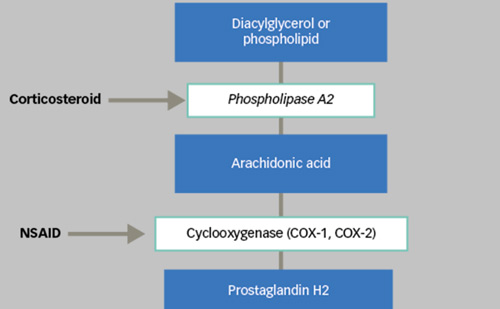
It should be no surprise that oxygen plays an important role in the treatment of an ischaemic disease. Diabetic retinopathy and retinal vein occlusions are ischaemic diseases, characterised by capillary nonperfusion and a lack of blood flow and oxygen. The ischaemic hypoxia stimulates the production of cytokines such as vascular endothelial growth factor (VEGF), resulting in neovascularisation and oedema formation. Traditional laser photocoagulation of the retina simply destroys some of the photoreceptors, reduces the oxygen consumption of the retina and re-establishes a balance between the oxygen supply and demand.
Pan-retinal Photocoagulation and Proliferative Diabetic Retinopathy
Traditionally, proliferative diabetic retinopathy has been treated with pan-retinal photocoagulation with a visible light laser. It is clinical practice to deliver mild to moderate laser burns that produce a light grey spot on the retina. Such a mild to moderate laser application will coagulate the retinal pigment epithelium and the adjacent photoreceptors, but leave the inner retina intact (see Figure 1).1 The photoreceptors use more oxygen than most cells in the body and destroying them is an effective way of reducing the oxygen consumption of the retina. A typical pan-retinal photocoagulation pattern of about 1,200–1,500 burns of 0.5mm diameter may reduce the number of photoreceptors and the oxygen consumption of the outer retina by approximately 20%.
It should be borne in mind that diabetic retinopathy predominantly involves the inner retina. This means that we must explain how coagulating cells and destroying oxygen consumption in the outer retina influences the inner retina. The explanation for this is found in the dual circulation and oxygen supply to the retina. The majority of the oxygen supplied to the retina comes from the choriocapillaris and diffuses into the outer retina, where it is consumed by the photoreceptors.
Usually, there is either an oxygen tension minimum in the middle of the retina2 or an oxygen watershed between the inner and outer retina. Normally, oxygen from the choroid does not reach the inner retina in humans; however, this is no longer true if the photoreceptors have been destroyed and the outer retinal oxygen consumption dramatically decreased. The oxygen flux from the choroid can now penetrate the outer retina without being consumed and can reach the inner retina, where it elevates the oxygen tension3–7 and improves hypoxia8 (see Figure 2).
This was initially shown by Stefánsson et al. in 19815 and was recently confirmed by Budzynski et al.9 This extra supply of oxygen to the inner retina compensates for the reduced supply by the retinal circulation. Hypoxia is corrected and the production of hypoxia-induced cytokines such as VEGF is normalised (see Figure 3).10,11
Hypoxia is the natural stimulant for VEGF, and neovascularisation and correction of this hypoxia by laser treatment is a perfect way to stop this process.
Starling’s Law and Macular Oedema
The development of macular oedema adheres to the principles of Starling’s law,12 as does, in general, vasogenic oedema. On the one hand, the increased permeability of the retinal vessels is produced by hypoxiainduced VEGF, which leads to the leakage of osmotically active molecules into the tissue, followed by water, i.e. oedema formation. On the other hydrostatic pressure in the capillaries and venules and increases the water flux from vessel to tissue.
Laser treatment and increased oxygenation affect macular oedema through these two different mechanisms.13 First, reduced hypoxia will decrease the production of VEGF and decrease vascular permeability. Second, autoregulatory arteriolar constriction decreases then hydrostatic pressure in the capillaries and venules, thus decreasing the flux of fluid from vessel to tissue and reducing oedema formation. By definition, oedema is an abnormal accumulation of water in a tissue and the development and regression of oedema is based on the movement of water between vascular and tissue compartments.14
Starling’s law describes the steady-state water exchange between the vascular compartment and the extra-cellular tissue compartment.15 Hydrostatic pressure in the vessel drives water into the tissue, and this is opposed by oncotic (osmotic) pressure differences between blood and tissue. Starling’s law holds that for an equilibrium in fluid exchange between the vessels and tissue, the hydrostatic and oncotic pressure gradients must be equal and opposite:
ΔP – ΔQ = 0
ΔP represents the hydrostatic pressure gradient and ΔQ the osmotic pressure gradient between the vascular and tissue compartments.
ΔP = πvessel – πtissue
πvessel is the hydrostatic pressure in the microcirculation and πtissue is the hydrostatic pressure in the tissue, which in the eye equals the
intraocular pressure.
ΔQ = θvessel – θtissue
θvessel is the osmotic pressure in the microcirculation and θtissue is the osmotic pressure in the tissue.
In the normal state these forces are in balance and there is no net movement of water between tissue and vascular compartments. If the osmotic pressure, θtissue, in the tissue is increased by a leakage of plasma proteins from the capillaries to the tissue compartment, ΔQ will decrease and oedema will result. This leakage and osmotic balance is controlled by VEGF, which is influenced by oxygen levels. Laser treatment that reduces hypoxia will reduce VEGF, the leakage and the osmotic pressure in the tissue, and thereby increase ΔQ and decrease the formation of oedema.
If the hydrostatic pressure, πvessel, in the capillaries and venules is increased, this drives water into the tissue and creates oedema, whereas decreased hydrostatic blood pressure, πvessel, would decrease oedema, assuming that the oncotic pressures are constant. The retinal arterioles serve as resistance vessels and control the hydrostatic pressure downstream. The diameter of the retinal arterioles is controlled by oxygen levels. In hypoxia, dilated arterioles have less resistance and consequently the blood flow and hydrostatic pressure, πvessel, is increased downstream in the capillaries and venules, where high hydrostatic pressure dilates these thin-walled vessels according to LaPlace’s law. The diameter of the arterioles and venules in the retina is an indication of the hydrostatic blood pressure in the retinal microcirculation. Prior to the development of diabetic macular oedema, the retinal arterioles and venules gradually dilate.16,17 Following macular laser treatment, the arterioles and venules constrict18 as the retinal oedema regresses. The same pattern is seen in branch retinal vein occlusion.19
Human Studies
Retinal oxygenation studies have traditionally involved invasive technology and, consequently, most studies have been conducted in experimental animals. However, two groups have used invasive oxygen tension measurements to study the oxygen effect of laser treatment in diabetic patients undergoing vitrectomy. Stefánsson et al.6 found a significantly higher oxygen tension over laser-treated areas than untreated areas in diabetic patients (see Figure 4), whereas Maeda et al.20 did not.
Recently,21 we developed a non-invasive spectrophotometric retinal oximeter that can be used clinically in human patients (see Figure 5). Using this device we have seen a significant increase in oxygen saturation in retinal blood vessels following laser treatment for retinal vein occlusions and diabetic retinopathy.22–25
There is also much indirect evidence to support the improved oxygenation following retinal photocoagulation in humans.26 It is well established that retinal blood flow and vessel diameters are inversely related to oxygen tension. High oxygen levels lead to vasoconstriction and lower blood flow.27 Feke et al.28 showed that retinal blood flow is reduced following pan-retinal photocoagulation in human diabetics, and this was confirmed by Grunwald et al.29 Fujio et al.30 elegantly showed that retinal blood flow was reduced in the half of the fundus treated with the laser compared with the untreated half. Wilson et al.31 used the original fundus photographs from the Diabetic Retinopathy Study (DRS) to measure the diameter of retinal arterioles and venules before and after pan-retinal photocoagulation. These vessels constricted significantly, by 10–15%, and there was also a significant correlation between the vasoconstriction and the regression of new vessels in the retina. Retinal vasoconstriction also
follows retinal photocoagulation for diabetic macular oedema18 and branch retinal vein occlusion.19 Kristinsson et al.17 demonstrated that retinal vessels dilate during the development of diabetic macular oedema32 and constrict following successful laser treatment (see Figure 6). Nguyen et al.13 studied the influence of oxygen on diabetic macular oedema in a direct way. Supplemental oxygen in breathing air reduced diabetic macular oedema over three months, and the oedema returned when the patients returned to breathing normal air.
Conclusion
The role of oxygen in ischaemic disease and its treatment is accepted in all fields of medicine. The role of oxygen in the therapeutic mechanism of retinal photocoagulation has been known for 27 years, and has been continually confirmed in experimental and clinical studies. The mechanism of retinal photocoagulation involves the oxygenation of the tissue,12 and improves the hypoxia induced by capillary non-perfusion or ischaemia. It reverses the consequences of hypoxia, i.e. VEGF formation and vasodilatation, new vessel formation and oedema.