Optic neuritis (ON) is an acute inflammatory condition affecting the optic nerve in young adults predominantly.1–4 It is caused by idiopathic inflammatory demyelination of the optic nerve, although there is also evidence of axonal loss.4,5 Its incidence amounts to 1–5 per 100,000 per year, being more frequent in Caucasians, countries at high latitudes and in spring.2,3,4,6 The patient’s complaints include both sudden, unilateral worsening of visual acuity ranging from mild visual disturbance to visual loss and movement induced ocular pain. Substantial female predominance among the patients is noted. ON is found to be a frequent initial manifestation of multiple sclerosis (MS), as up to 50 % of ON cases are likely to progress into MS within 15 years.1–4
Diagnostic Criteria
ON is a self-limiting condition, progressing over hours to 10 days and spontaneously improving within up to 8 weeks. Such a condition not presenting recovery within 8 weeks should require further investigation and may impose other diagnosis implementation.4ON can usually be diagnosed taking only clinical features in to consideration.2,3 Although, typical ON requires no further laboratory studies visual evoked potentials (VEP) testing,2,7,4 magnetic resonance imaging (MRI) is recommend for prognostic purposes.4 It was recently shown that patients with normal VEP and MRI had a 96 % probability of a normal lumbar puncture, thus both tests are suggested in all patients before deciding on a lumbar puncture.8
The most common presentation is a unilateral, subacute, painful visual loss, which is not associated with any systemic disease or other neurological symptoms. Visual acuity might deteriorate to zero light perception in the affected eye, but also can be as minor as blurry vision only. Other frequent clinical characteristics of ON include colour vision disturbance of a non-specific pattern, contrast sensitivity reduction, photopsias, relative afferent pupillary reflex (RAPD) and visual field loss presence.2,4,9 Pau et al. divided ON into four clinical categories, depending on the anatomic localisation:
- retrobulbar neuritis characterised by normal disc appearance;
- papillitis with swollen optic disc;
- perineuritis involving mainly the optic nerve sheath with or without optic disc oedema; and
- neuroretinitis with swollen optic disc and a ‘star figure’ of macular exudates.
The two first forms are most commonly associated with MS ON. Retrobulbar neuritis accounts for two-thirds of acute demyelinating ON. Temporal optic disc atrophy as well as other residual clinical findings are often seen after ON resolution.4 The ON recurrence ratio is described to reach 28 and 35 % at 5- and 10-year follow up respectively.10,11 Differential diagnosis encompasses hereditary, ischaemic, compressive, toxic and other inflammatory optic neuropathies.3
Treatment Trials
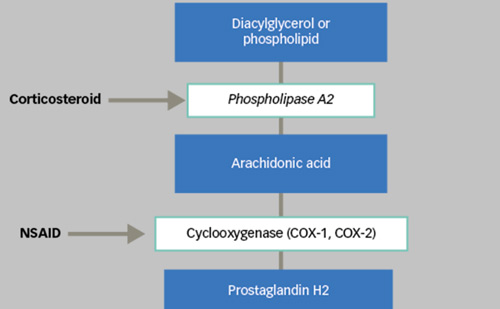
In the decades since its first clinical implementation in the 1950s, corticosteroids proved useful in dealing with ON as well as MS.12 Many clinical trials have been conducted to establish an optimal therapeutic regimen and asses treatment efficacy and its indications.1,7,9,10,12–22 The trial including greatest number of patients, which became leading treatment guideline, was the Optic Neuritis Treatment Trial (ONTT), carried out in 1988–2006.1,2,9–12,15,18
Table 1: Treatment Trials of Optic Neuritis
Optic Neuritis Treatment Trial
The ONTT was a prospective randomised trial enrolling 389 patients with acute ON, presenting up to 8 days after onset of the initial episode. The trial evaluated MS risk after an episode of ON and factors predicting of high and low risk under three corticosteroid concerning therapeutic approaches: 3-day course of methylprednisolone given intravenously in a dose of 250 mg every 6 hours followed by 2 weeks of daily oral prednisolone in a dose of 1 mg/kg/day, oral prednisolone alone in a dose of 1 mg/kg/day for 2 weeks and placebo. Yearly neurological and ophthalmological examinations were conducted within the first 5 years after inclusion, then 5 and 10 years later. Visual acuity, contrast sensitivity, colour vision and visual field were tested during the ophthalmological exam.1,2,12,15,18 The final follow-up evaluation showed that intravenous corticosteroids followed by oral corticosteroids ensured lower risk of MS occurrence as well as improved visual recovery period but had no impact on final visual outcome.1,7,9,12 Interestingly, a smaller rate of recurrence within first 2 years following the first episode of ON wasdescribed in above-mentioned treatment group compared to oral corticosteroids assigned group as well as placebo group. The beneficial effect of intravenous methylprednisolone treatment on the development of MS lessened after 2 years.1,7,9,10,12 By five years, the treatment had no significant effect on the development of MS, reported Beck et al.12
The ONTT showed that 15-year risk of developing MS was 50 % regardless of the treatment regimen. The risk was strongly dependent on the MRI findings at the onset. In subjects presenting with at least one pre-existing white matter demyelination lesion in brain MRI the risk was substantially higher, reaching a rate of 72 %, while the MS development ratio in patients with normal brain MRI at the initial ON episode amounts to 25 %.1,7,12 For patients with no white matter lesions at presentation the greatest MS development risk was shown to occur in the first 5 years after initial ON, approximating zero later than 10 years after onset.1,7,12,18 In the group with positive MRI readings the MS development risk did not vary with time within the 15-year observation period, nor increased with additional lesions appearance.1,7 According to ONTT, MRI remains a single most important predictor of risk of developing MS.1,7,18 MS was more frequently encountered in patients with retrobulbar ON and in cases with absence of atypical findings such as no light perception at presentation, absence of ocular pain, severe optic disc swelling, peripapillary haemorrhages or retinal exudates.
Corticosteroids are a powerful group of medicines, causing potentially serious side effects. However, infrequent major side effects were reported in ONTT, including psychotic depression and pancreatitis, which improved with no sequelae after cessation of the treatment. The minor side effects described in the study listed insomnia, mild mood changes, stomach upsets, facial flushing, acne, oedema and weight gain.1,7,12 The clinical findings scope of the ONTT revealed relatively frequent fellow eye abnormalities – found in one of four tested parameters in 67 % of patients, arguing for bilaterality of the condition. The most sensitive measure of residual visual disturbance was contrast sensitivity test being the most consistently abnormal in post-ON patients.7
Citing after Kaufman et al., several questions concerning future ON corticosteroids treatment research emerge: whether corticosteroid treatment is beneficial in patients whose symptom duration is longer than 8 days; whether larger doses of corticosteroids are more effective than lower doses; what the optimal corticosteroid regimen is; whether the observed increased ON recurrence rate associated with oral prednisone is also observed in MS attacks; and whether high-dose methylprednisolone given periodically will improve the prognosis for patients with MS.3
Immunomodulatory Treatment
Disease-modifying agents are regarded as delaying progression of the disease, increasing the time delay to the second clinical episode and modulating disease course by diminishing the frequency of MS episodes. Such drugs as interferon beta-1a and interferon beta-1b are known to be beneficial in immunomodulatory treatment of ON and MS.2,14,16,17,19,23 It is important to underline that patients will need to undergo treatment for approximately 6 years to prevent a relapse and that a brain MRI is required at therapy initiation for a proper prognosis evaluation and treatment monitoring.2,13 Several multiple, randomised, double-masked, placebocontrolled trials have looked at the utility of these immunomodulatory agents in patients with a clinically isolated syndrome (e.g., ON) and at least two or more white matter lesions on brain MRI.2,14,16,17,19
Controlled High-risk Avonex Multiple Sclerosis Prevention Study
The Controlled High-risk Avonex Multiple Sclerosis (CHAMPS) study was established to verify whether beta interferon delays the progression from clinically isolated syndrome (CIS) suggestive of MS, e.g. ON, to clinically definite MS. Inclusion criteria included occurrence of first demyelinating event and presence of two or more clinically silent brain lesions on MRI. Intramuscular injections of 30 μg of interferon beta-1a were given once a week and compared to placebo injections in a group of total 383 patients. The study was interrupted at 3 years’ follow up, having shown an important reduction in probability of MS development in interferon group compared to placebo group.16,19
Balcer et al. report that, although the potential for long-term benefit of interferon beta-1a in high-risk patients with acute monosymptomatic demyelinating ON is not known, data from CHAMPS provide rationale for early therapy.23
Early Treatment of Multiple Sclerosis Study
Similar results were obtained in the Early Treatment of Multiple Sclerosis (ETOM S) study, comparing weekly subcutaneous injections of 22 μg of interferon beta-1a to placebo through 2 years. The interferon treatment proved to be well tolerated with no major side effects, supporting initiation of early interferon beta-1a therapy in patients with acute ON or other first high-risk demyelinating event.16,17
Betaferon in Newly Emerging Multiple Sclerosis for Initial Treatment Trial
The Betaferon in Newly Emerging Multiple Sclerosis for Initial Treatment (BENEFIT) trial investigated the effect of treatment with interferon beta-1b after a clinically isolated syndrome. As described by Kappos et al. patients with a first event suggestive of MS and a minimum of two clinically silent lesions in MRI were randomly assigned to receive interferon beta-1b 250 μg (n=292; early treatment) or placebo (n=176; delayed treatment) subcutaneously every other day for 2 years, or until diagnosis of clinically definite MS. The findings of this trial were consistent with those reported by earlier studies, arguing for an early initiation of treatment with interferon beta.14
Acute Optic Neuritis Treatment Guidelines
The treatment regimen in the acute ON remains a controversial topic in current neuro-ophthalmology.1,3,23 The ONTT recommends not administering corticosteroids in case of first episode of a monosymptomatic ON with no pathological findings in brain MRI. In the clinical practice a more convenient than reported in ONTT therapeutic regimen has been adopted, however untested and unproven. It opts for a single dose of 1 g of methylprednisolone sodium succinate for 3 days, enabling out-patient treatment implementation.2,7
Treatment with oral prednisolone in standard doses is contraindicated in the treatment of acute ON due to increasing the recurrence rates of ON .3,7,12 Intravenous immunoglobulin and plasma exchange have not proven potent enough to be recommended on a routine basis.20,21,22 Small sample clinical trials proving that the use of the adrenocorticotrophic hormone (ACTH) may hasten the speed and degree of recovery of visual function in persons with acute monosymptomatic ON have been conducted, although their implementation in the clinical practice is far from being vast and profound.3,24
Provided that there is lack of long-term follow up studies, Kaufman et al. recommend that the decision to use the aforementioned medications to speed recovery but not to improve ultimate visual outcome should be based on other non-evidence-based factors such as quality of life, risk to the patient, visual function in the fellow eye or other factors that the clinician deems appropriate.3
Conclusion
ON is a common self-limiting inflammatory condition affecting optic nerve, linked with high risk of developing MS. It causes mild to important visual disturbances which usually recover without treatment. Multiple clinical trials have been conducted in order to establish the treatment guidelines for acute ON, although the treatment approach remains controversial and requires further investigation including large group, long-term follow up studies.