Age-related macular degeneration (AMD) is the leading cause of severe visual acuity (VA) loss in industrialised countries and its prevalence is increasing with the aging population.1,2 There are two forms of the disease – dry AMD and exudative AMD. Dry AMD is associated with drusen early on, followed by atrophy of the macula during the later stages. Exudative AMD is associated with the development of a choroidal neovascular membrane (CNV), which causes fluid exudation or hemorrhage in the macula. Although the pathogenesis of the disease is still under investigation, genetic predisposition, age, ischaemia, and environmental factors all have a role in its development.3,4
The vitreous is a clear gel that is attached anteriorly at the vitreous base and posteriorly to the optic nerve, macula and blood vessels. With time, vitreous degeneration occurs, which subsequently leads to contraction and separation from the macula and optic nerve (known as posterior vitreous detachment or PVD). Vitreomacular adhesion (VMA) has been related to several macular diseases, including vitreomacular traction syndrome, diabetic macular oedema, macular hole and epiretinal membrane. The concept of the pathogenesis of macular degeneration based solely on a retinal pigment epithelium (RPE) disease has left many questions unanswered and, hence, the role of the vitreous and its adherence to the retina in exudative AMD has recently been studied. This review provides a critical discussion of current scientific evidence of the role of the vitreous in the pathogenesis of exudative AMD.
Posterior Vitreous Adhesion and its Relationship with Exudative Age-related Macular Degeneration
Traditionally, the vitreous has not been associated with exudative AMD. However, recent studies have shown that the posterior hyaloid might have a role in the pathogenesis and progression of the exudative form of AMD.
A high incidence of posterior vitreous attachment was recently observed intra-operatively in patients with exudative AMD.5 Schmidt et al. also observed that intra-operative findings during vitrectomy showed little liquefaction of the vitreous gel, an incomplete PVD, and remarkably firm attachments at the macula in all patients with AMD in their series (10/10).6 Studies using ultrasound suggest that complete PVD occurs less frequently in eyes with AMD compared with age-matched controls, and that a higher incidence of VMA is detected in both exudative and non-exudative AMD.7,8 Other studies have shown that an attached posterior vitreous cortex, partial peripheral PVD, and central adhesions surrounded by shallow detachment of the posterior vitreous cortex were significantly more frequent in exudative AMD than in non-exudative AMD and control eyes.9,10
VMAs were described in one study in 36 % of eyes with exudative AMD, significantly more frequently than in eyes with non-exudative AMD or control eyes.9 These results were confirmed by Robison, who found VMA in 38 % of eyes with exudative AMD,10 and by Lee,11 who found VMA in 22.3 % of eyes associated with neovascular AMD.
Optical coherence tomography (OCT) is a non-invasive method that provides micron-resolution, cross-sectional imaging that is useful in imaging the retina and vitreoretinal interface. Conventional time-domain OCT has been used to evaluate the vitreous in AMD, and such studies have suggested that there is a higher rate of VMA in exudative AMD, whereas no difference was found between non-exudative AMD and normal populations.9 Similarly, using spectral domain OCT combined with simultaneous scanning laser ophthalmoscope (spectral OCT/SLO), Mojana et al.12 demonstrated posterior hyaloidal adhesion in 170 eyes with AMD, which frequently caused VMT in eyes with CNV. In their study, exudative AMD had a significantly higher incidence of incomplete PVD compared with age-matched control eyes, and a similar trend existed when comparing non-exudative AMD eyes with the control group. However, there was no correlation between the size of the hyaloid attachment and the area of the CNV complex in their study. Krebs et al.13 studied the vitreoretinal interface using spectral domain OCT in 30 eyes with exudative AMD and VMA, and found that the localization of the adhesion corresponded in 100 % of cases with the area of the CNV and, in 83.3 % of cases, traction towards the optic disc could be seen.13
Lee et al.14 studied patients with unilateral exudative AMD, and found that CNV was present in 83 % of eyes with VMA (44/53 eyes) and in 11 % of eyes without VMA (6/53 eyes), which was statistically significant. The location of VMA was always observed over the area of the CNV in exudative eyes in their study, suggesting that traction from the posterior hyaloid is responsible for the development of the CNV lesion.
Robison et al.10 compared 29 previously untreated subjects with active exudative AMD in one eye and non-exudative AMD in the fellow eye, with 10 previously untreated subjects with end-stage geographic atrophy in one eye and an end-stage fibrotic (disciform) scar in the fellow eye. Subjects were studied using ultrasonography to identify the presence of PVD and using OCT to detect VMA. The incidence of PVD in eyes with non-exudative AMD was 20/29 (69 %), compared with 6/29 (21 %) with active exudative AMD. VMA was present in 11/29 eyes (38 %) with exudative AMD and in only 3/29 eyes (10 %) with non-exudative AMD. The incidence of PVD in geographic atrophy was 7/10 (70 %), compared with 4/10 (40 %) with disciform scar (p=0.44). VMA was present in 2/10 (20 %) eyes with disciform scars and in 0/10 (0 %) eyes with geographic atrophy (p=0.48). The authors concluded that PVD might protect against exudative AMD, whereas VMA might promote exudative AMD. This phenomenon was not evident in end-stage disease because of an increased incidence of PVD and a decreased incidence of VMA in eyes with disciform scars.
Nomura et al.15 performed a retrospective study involving 378 eyes with typical AMD, polypoidal choroidal vasculopathy (PCV), and control eyes. PVD and VMA were investigated by ultrasonography and SD-OCT, respectively. In typical AMD eyes, the frequency of complete PVD was significantly lower (57 %) than in the controls (70 %), and the frequency of VMA tended to be higher (12 %) in typical AMD eyes than in the controls (7 %). In patients with unilateral exudative AMD, the frequency of complete PVD was lower in typical AMD eyes than in fellow eyes. Lambert et al.5 found an attached vitreous in 8/10 patients (80 %) with CNV, and speculated that VMA induces mechanical traction that contributes to CNV progression.
There is also some evidence that the treatment outcomes for exudative AMD are affected by posterior hyaloid adhesion. Lee et al.16 compared the visual outcome of anti-vascular endothelial growth factor (VEGF) treatment for exudative AMD with or without posterior VMA in 148 patients. They found that posterior VMA was associated with an inferior visual outcome after intravitreal anti-VEGF treatment for exudative AMD. The authors documented posterior VMA using StratusOCT™ and concluded that chronic tractional forces might antagonize the effect of anti-VEGF treatment, resulting in a poor response to anti-VEGF treatment in patients with VMA.
Sakamoto et al.17 studied the effect of pars plana vitrectomy (PPV) on CNV in 92 eyes with AMD and vitreous haemorrhage, and found that the activity of CNV was reduced in 74 % of eyes and that VA significantly improved. This suggested that the vitreous and interactions between the vitreous and the retina have a role in exudative AMD.
Another study18 of a subpopulation of exudative AMD also found that vitrectomy was beneficial in visual improvement, possibly from the release of VMT and improvement of retinal oxygenation. The study also concluded that the compressive effect of gas might facilitate reabsorption of the intraretinal fluid. However, the authors correctly stated that surgery in such eyes can result in complications, and that vitrectomy might also complicate anti-VEGF treatment. This is because it can shorten the half-life of intravitreal anti-VEGF drugs, so that higher doses of anti-VEGF drugs might be needed post-operatively.18 There are more reports of CNV regression after surgery for exudative AMD. Vitrectomy was performed in 12 eyes from 11 patients with highly active CNV, in whom the posterior vitreous surface remained attached. Six months after surgery, CNV disappeared completely in two eyes and showed regression in six eyes.19
Proposed Mechanisms of Development of Exudative Age-related Macular Degeneration in Patients with Vitreomacular Adhesion
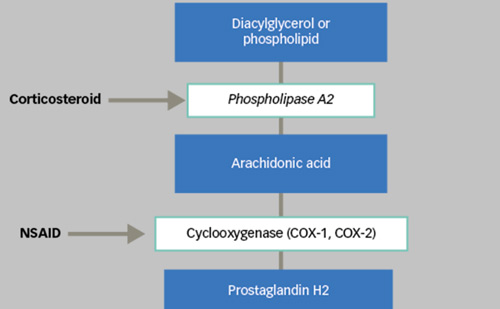
The mechanism by which VMA exacerbates exudative AMD is uncertain, and multiple theories have been proposed, including – mechanical forces worsening macular oedema, persistent VMA inducing chronic low-grade inflammation, preventing normal oxygen and nutrients diffusion to the macula, and/or confinement of pro-angiogenic cytokines near the macula. Anterior–posterior forces, present at the surface of the retina, might exacerbate the macular edema created by the leaking vessels in the CNV complex. Some authors have hypothesised that increased mechanical forces associated with abnormal vitreal attachments might result in the secretion of signaling factors by the Müller cells, with both paracrine and autocrine effects. This process can lead to a cascade of inflammatory factors and local vascular changes, which include vascular leakiness, and subsequent cystoid macular oedema (CME).20 In turn, in eyes with CNV, this could set up a vicious cycle, in which the inflammation, the reactive gliosis, and the tractional forces might result in worsening of the chronic exudation of the underlying disease.
In eyes that have a pre-existent PVD, the disruption between the retina and the vitreous might enable liquefied vitreous to flow freely across the retina, aiding in toxin removal and oxygen exchange. However, if the posterior vitreous is still intact, it is speculated that degeneration of the retina occurs owing to the lack of nutrient and oxygen exchange, thus leading to exudative AMD.
Persistence of hyaloid adhesion to the posterior pole is associated with AMD. This adhesion is often responsible for VMT in eyes affected by exudative AMD. Mechanical factors related to the traction forces might antagonize the effect of anti-VEGF treatment, thus being responsible for pharmacological resistance in a subpopulation of patients with AMD.
Conclusions
It is likely that vitreomacular traction alone is not able to induce AMD. It is more likely that the fundamental pathomechanism of AMD formation must have already begun for tractional forces to achieve a change for the worse. The high coincidence of vitreomacular traction and CNV, as well as the observable success of vitrectomy in other diseases of the vitreoretinal interface, should lead physicians to consider vitreous changes when diagnosing and treating patients with AMD. ■