Descemet membrane detachment (DMD) is a well-described complication following a wide range of intraocular surgeries and is most commonly reported following cataract surgery.1 DMD has been observed after vitrectomy, penetrating keratoplasty and trabeculectomy procedures, among others.2 Several cases of DMD have also been described following use of intracameral viscoelastic injections for hypotony after trabeculectomy and glaucoma tube implants.3,4 Lower endothelial cell density and presence of corneal guttata have been identified as risk factors for DMD during cataract surgery.5 Several other factors, such as mutations in the gene encoding transforming growth factor-β, shallow anterior chambers and the use of dull surgical instruments, have also been implicated as risk factors for DMD during cataract surgery.1 Despite these associated DMD risk factors following cataract surgery, the risk factors for DMD following glaucoma surgery are not well described in the literature and there are no previous case reports of DMD following gonioscopy-assisted transluminal trabeculectomy (GATT).
GATT is a micro-invasive glaucoma procedure first described by Grover et al. in 2014 and has been shown in subsequent studies to be a safe and effective therapy for primary, juvenile and secondary open-angle glaucoma.6–8 A fibre-optic coaxial catheter is often used in GATT and allows the simultaneous visualization of the catheter tip position and viscodilation of the Schlemm canal. In a 24-month follow-up study that included 198 patients, Grover et al. documented a single case of DMD following GATT, but there were no proposed mechanisms or structural imaging of the detachment.6 Herein, we report two cases of DMD following GATT procedures performed at Bascom Palmer Eye Institute, University of Miami, in patients with open-angle glaucoma and histories of intravitreal injections of anti-vascular endothelial growth factor (VEGF) agents. Currently, the use of GATT in patients with a history of retinal neovascularization and multiple intravitreal anti-VEGF injections is not documented in the literature.
Case presentations
We present two cases of ab-interno canaloplasty with 360-degree GATT performed in the setting of glaucoma with previous retinal vein occlusion, which were complicated by DMD. In both cases, the DMD was not noted at the time of surgery but was identified on postoperative day 1. Again, in both cases, the DMD was not connected to the corneal incision but rather to other portions of the anterior chamber angle. These cases were followed without intervention and both resolved spontaneously. We postulate that the history of neovascular processes in these cases possibly played a role in increasing the risk for DMD associated with GATT.
Case 1
A 28-year-old woman was referred to our institution from an outside ophthalmologist. She had a history of central retinal vein occlusion in both eyes and uncontrolled intraocular pressure (IOP) in both eyes over the course of the previous year. She had received multiple intravitreal ranibizumab injections in both eyes in her home country. The patient was diagnosed with juvenile open-angle glaucoma (JOAG) in the right eye, with a severe inferior visual field defect threatening fixation, as well as suspected JOAG in the left eye due to elevated pressure, cupping and nerve fibre layer changes. Her ophthalmic history also included pathological myopia and stromal infiltrate secondary to a previous viral conjunctivitis in both eyes.
In May 2018, the patient underwent uncomplicated GATT in her right eye, which lowered the IOP substantially from 38 to 15 mmHg. A decision was made to perform GATT in the left eye as well. The left eye preoperative visual acuity (VA) was 20/40 and IOP was 22 mmHg. The technique for GATT used in this case included a corneal paracentesis created at the 6 o’clock meridian, followed by intracameral injection of carbachol for pupillary constriction, and ocular viscosurgical device (OVD)-aqueous exchange to maintain the chamber depth. The illuminated microcatheter (iTrack; Nova Eye, Inc., Fremont, CA, USA) was primed, tested and introduced into the anterior chamber through the paracentesis. A temporal clear-corneal wound was created, and the microscope was tilted away from the patient for gonioscopy visualization. Under direct gonioscopic visualization, the nasal angle was incised using a 25-gauge microsurgical blade to create a goniotomy. The illuminated microcatheter was grasped by intraocular forceps and the catheter tip was introduced through the goniotomy to cannulate the Schlemm canal. The catheter was advanced with slow injection of OVD. Once the tip of the catheter emerged from the goniotomy, it was grasped with the intraocular forceps and a circumferential trabeculotomy was created in a purse-string fashion. OVD was washed out from the chamber and surgical wounds were closed using dissolvable polyglactin sutures. A 360-degree goniotomy was achieved and no DMD was noted by the operating surgeon at the end of surgery, although refluxed blood in the anterior chamber partially obscured the view.
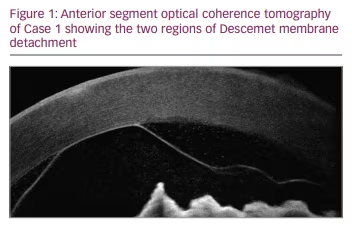
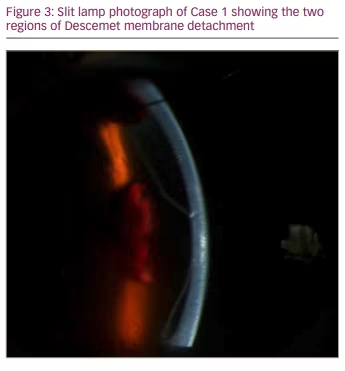
On postoperative day 1 after GATT in the left eye, the patient’s VA was 20/150 and IOP was 15 mmHg. Two separate lobulated DMDs were noted on examination, one inferior and one superior, along with stromal infiltrates, haze, oedema and blood between the Descemet membrane and the stroma. Neither detachment appeared connected to the corneal incision. Anterior segment optical coherence tomography (OCT) images (Figure 1) were obtained along with slit lamp photographs (Figure 2, Figure 3). The patient was evaluated by a cornea specialist and it was decided that observation was the best initial strategy in the treatment of this patient and the patient was monitored without immediate intervention for the DMD.

At the week 1 postoperative visit, the patient was seen again by a cornea specialist and the DMD was noted to be much less bullous. Three weeks following GATT, the DMD was noted to be improving, with the inferior detachment nearly completely resolved. At approximately 6 weeks postoperatively, the DMD had resolved, with a small area of fibrosis of the stroma inferiorly. The VA was 20/80 and the IOP was 17 mmHg, and the patient was advised to follow up with her ophthalmologist in her home country. An update from the overseas ophthalmologist approximately 1 year later indicated a best corrected VA of 20/25 with no DMD, and IOP controlled on no medications.
Case 2
A 75-year-old man presented to our institution with pain and decreased vision in the right eye. His right eye VA was 20/200 and IOP was 45 mmHg. His pressure was lowered into the 30s with several rounds of drops. The patient was diagnosed with neovascular glaucoma secondary to a central retinal vein occlusion and was administered intravitreal bevacizumab. Within a week of his initial presentation, the patient underwent panretinal photocoagulation and was followed for an additional month with controlled IOP but with no improvement in VA before being lost to follow-up for approximately 8 months.
The patient presented again the following year with pain and decreased vision to hand motion (HM) in the right eye. The patient was followed in clinic for several visits over a 12-week period, with IOPs ranging from 32 to 44 mmHg and refractory to medical therapy. His angles remained open without overt neovascularization, and a decision was made to perform GATT with viscodilation of the Schlemm canal in the right eye. At the time of surgery, the patient’s right eye VA was HM and IOP was 34 mmHg. In May 2018, the patient underwent GATT with an illuminated microcatheter as described above, with no unexpected findings or complications at the time of surgery. A 360-degree cannulation was achieved and no DMD was noted by the operating surgeon at the end of surgery, although refluxed blood in the anterior chamber partially obscured the view.
At the day 1 postoperative visit, the patient’s VA was HM and IOP was 9 mmHg. The operating surgeon noted a possible DMD at this visit, inferior to, but not connected with the temporal wound created for the goniotomy blade, along with blood in the anterior chamber. It was decided that the best course of action was to observe the possible DMD for spontaneous improvement. A stable DMD was confirmed outside of the visual axis at the week 1 follow-up visit. The DMD was noted to be improving at week 3, and by 5 months postoperatively, the DMD was no longer noted. The patient’s vision remained stable at HM and IOP was 21 mmHg.
Discussion
GATT has been shown to be a safe and effective procedure for control of IOP and provides another option for surgeons and their patients to lower IOP without the creation of an extraocular aqueous reservoir. This case report demonstrates that DMD is a rare but potentially sight-threatening complication of GATT, which has not previously been described in detail. In the two cases presented here, it is unknown whether the history of neovascularization and/or the history of anti-VEGF injections contributed to the DMD. One hypothesis is that during GATT, viscodilation of the Schlemm canal can result in the separation of the Descemet membrane from the stroma if the viscoelastic were to dissect into the potential space between the two layers. Alternatively, during circumferential trabeculotomy, when pulled in a purse-string fashion, the cannulating filament may result in partial or complete DMD if the cleavage plane is anterior to the trabecular meshwork (TM). Some eyes may have a fibrotic TM due to a history of chronic inflammation of regressed neovascularization. In these cases, the fibrotic TM may have a higher resistance to rupture when viscoelastic is injected, making the Descemet–stroma interface the path of least resistance and placing these patients at higher risk of DMD. While there are many published reports on the safety and efficacy of GATT in different types of glaucomas, including steroid induced9 and primary angle closure,10 there are no reports specifically on the use of GATT in the setting of neovascularization.
DMD can be left for observation or managed surgically depending on the nature of the detachment.11 The two cases presented here demonstrate spontaneous reattachment with resolution or near-complete resolution within 6 weeks of presentation for these planar detachments involving OVD.
A potential limitation of this report is the lack of more long-term follow-up on these patients; however, in both cases, the DMD was noted to be resolved by the point of last follow-up several months after surgery. Spontaneous reattachment is less common in non-planar DMD and in cases where the membrane scrolls. Even in planar DMD without scrolling, the timing and probability of reattachment can be unpredictable according to previous reports.2 A case series of DMDs after cataract surgery showed a 53% reattachment rate within 20 weeks of the initial operation in patients with non-scrolled detachments.2 In more severe detachments or those that do not self-resolve, surgical options such as air bubble injection into the anterior chamber or descemetopexy may be used.12
Conclusion
In the two cases that we share in this article, both DMDs self-resolved within several weeks and did not further complicate the management of the patients’ glaucoma. However, these two cases illustrate that DMD is a potential complication of GATT in the setting of previous anti-VEGF treatment and patients undergoing these procedures should be monitored closely after surgery.







