Case Report
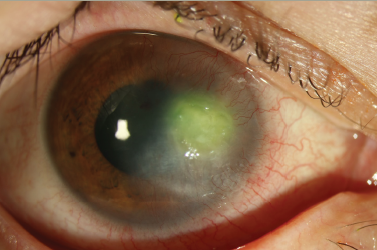
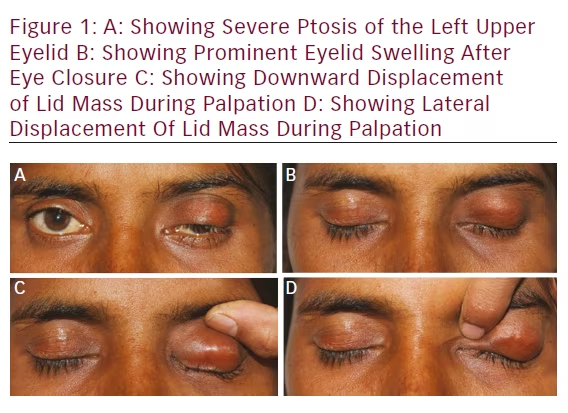
A healthy 25-year-old female patient, with a 6-month history, reported with a chief complaint of left upper lid mass and droopiness. History revealed that the swelling initially started as a peanut size and had gradually increased to the present size. Ocular examination was suggestive of nontender, bony hard, noncompressible, nonfluctuant, and nonpulsatile swelling on the left upper lid (see Figure 1A and B). The superior, inferior, medial, and lateral margins were well palpable. Mass was nonadherent to orbit, and it could be digitally displaced horizontally or vertically (see Figures 1C and D). The size of the swelling was 25 × 15 × 10 mm.
There was a history of blunt trauma to the left upper lid, and 3 months before she noticed this swelling. There was no history of vision changes, ocular pain, pain with eye movement, or headaches. Her vision was 20/20 in both the eyes. Both the eyes underwent slit lamp examination and fundus was also normal.
Past ocular history and medical history were noncontributory.
Review of systems was negative.
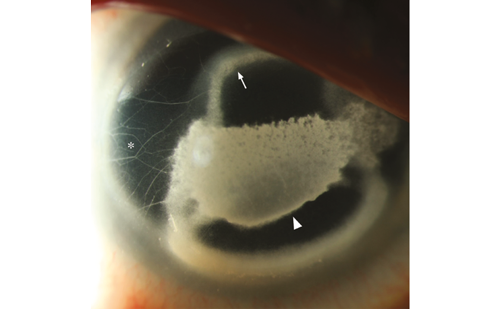
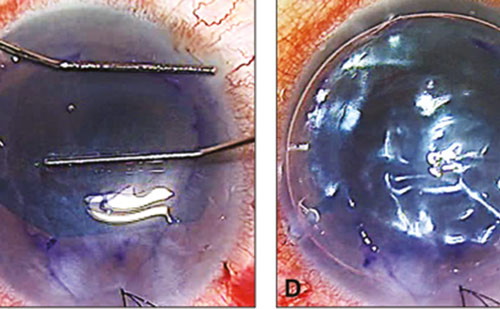
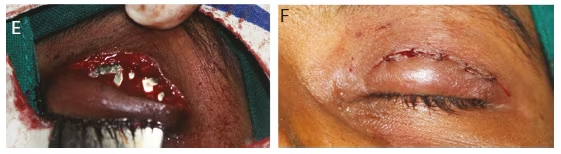
The patient was operated under local anesthesia. Two silk sutures were taken near the lid margin to provide traction during surgery. The globe was secured with an entropion plate. Lid crease incision was performed superficial to tumor (see Figures 2A and B). The lesion was isolated from the surrounding tissue by blunt dissection. Dissection was easily carried out around the mass except for the lower portion, which was found adherent with tarsal plate (see Figures 2B–D). The tumor and its extent were identified. The lesion was excised completely (see Figure 2E). No communication with the orbit or sinuses could be identified.
The tarsal plate was sutured with 6-0 vicryl interrupted sutures. Skin was sutured with interrupted 6-0 vicryl sutures (see Figure 2F). Patient’s ptosis was mostly recovered on 14th postoperative day (see Figure 3B). Specimens sent for histopathologic examination and histopathologic findings were consistent with an osteoid osteoma.
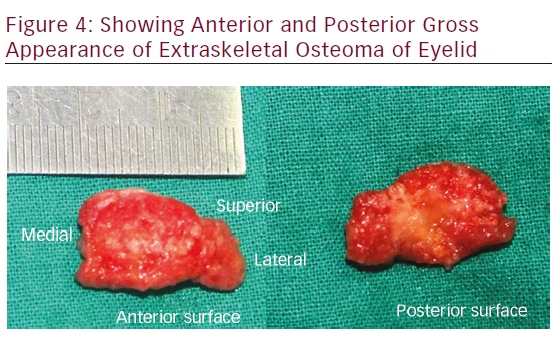
Gross Examination
The tumor was an encapsulated nodular lesion 25 × 15 × 10 mm in size. The consistency was bony hard. The anterior surface was glistening— white to pink color and was smooth with rounded protuberance. The cross-sections of specimen could not be cut by scalpel (see Figure 4).
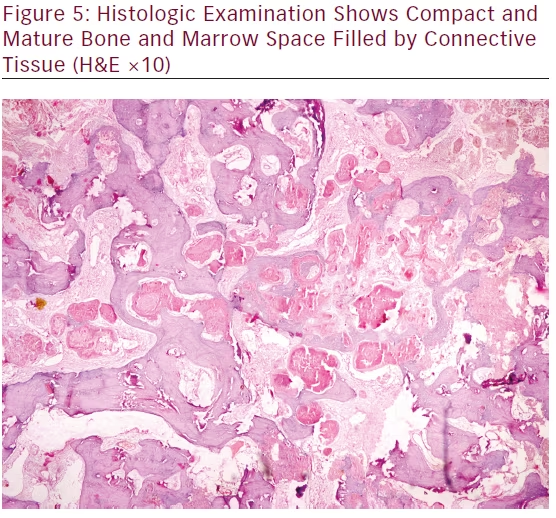
Microscopic Examination
Histologic examination shows compact and mature bone and marrow space filled by connective tissue (see Figure 5).
Discussion
Osteoma is a benign slow-growing osteogenic lesion, composed of well-differentiated mature bone tissue, characterized by the proliferation
Trauma and Surgery

of compact or cancellous bone, almost exclusively found in the head and neck region. Central, peripheral, and extraskeletal are the three variants of osteoma. Trauma, inflammation, developmental disorders, and genetic defects are considered as the etiologic factors.1
Osteoma can occur at any age, but more frequently seen between the third and fifth decades. It has got a slight male predilection.2 Paranasal sinuses are the favorite locations of peripheral osteoma of the craniofacial region—frontal and ethmoidal sinuses being the common ones. External auditory canal, orbit, temporal bone, and pterygoid processes are the other locations.3 Primary orbital bone tumors constitute a very small percentage of all orbital tumors. More often, osteomas originate from the paranasal sinuses. Among the bony orbital tumors, fibrous dysplasias and osteomas are the most commonly encountered entities.4
The case we reported here was an extraskeletal osteoma of the eyelid, as it was located in the left upper lid without any communication to orbit or
paranasal sinuses. There was a history of blunt trauma to the left upper lid 3 months before this lid mass was noticed by the patient. The extraskeletal soft tissue osteoma usually develops within the muscle. In our case, extraskeletal osteoma probably was developed from orbicularis oculi of the left upper lid. During surgery, we found that this lesion was lying just beneath pretarsal muscle and anterior to tarsal palate. It was confined only to the eyelid. Extraskeletal osteoma of the lid is very rare. To the best of our knowledge, this is the first case of extraskeletal osteoma of the lid reported in the English language literature.
The osteoma is often slow growing and asymptomatic, diagnosed incidentally on radiographs. But later on, it can achieve a faster growth rate, as the rate of osteogenesis increases, and can cause deformation of the bone and compression of the adjacent structures. They usually appear
as unilateral, sessile or pedunculated, well-circumscribed, mushroomlike masses, ranging from 1.5 to 40 mm in diameter.5 All these features are consistent with the present case. During physical examination, tumor was confined to eyelid and boundaries were well defined and palpable. So we did not order for computed tomography scan and planned this case for an excisional biopsy.
The differential diagnoses in this case include osteoid osteoma, dermoid cyst, and lipoma. Osteoma of the orbit can be seen as a bony hard swelling.6 Dermoid cyst and lipoma are also seen as subcutaneous nodules in the lid, but they will be soft and fluctuant.7
Management of osteoma of the eyelid is complete excision with clear margin to establish the histopathologic diagnosis and prevent recurrence.