Dry Eye Classification
The arena of dry eye disease (DED) has become its own area of expertise, requiring a thorough knowledge of the etiologic, diagnostic, and therapeutic options and approaches in order to achieve a pristine ocular surface. There are various reports indicating that up to 25–30 million Americans suffer from dry eye, with at least 50 % of the patients visiting eye care professionals for at least a primary or secondary complaint of dry eye.1 A Gallup survey in 2012 further showed that the majority (66 %) of patients seen at a formal eye exam level have tried three or more artificial tears for 2 or more years prior to the exam.2 The definition of DED has changed from the original Pflugfelder definition in 20043 where the lacrimal unit created a dysfunctional tear film to that of the International Delphi Panel in 2007 creating the new DEWS definition: dry eye is a multifactorial disease of the ocular surface resulting in discomfort, visual disturbance, and tear film instability accompanied by increased inflammation and osmolarity of the tear film and ocular surface.4
The tear film is the most important refracting surface of the eye and is really a complex interaction of the environment, the aging process, systemic diseases, systemic medication, osmolarity, inflammatory processes, and lacrimal gland neuroregulation. As a result of these interactions, ocular surface abnormalities are clinically relevant as crossover or combination of evaporative dry eye (posterior blepharitis, meibomian gland dysfunction [MGD], or lid margin disease), aqueous deficiency (dry eye syndrome or primary/secondary Sjogren’s syndrome), and/or ocular allergy. Posterior blepharitis/MGD is a chronic, recurrent, and progressive disease of the meibomian glands of the eyelids (lower greater than upper) and can be obvious (plugged meibomian glands, gland dropout, or inflammation on slit lamp evaluation), or non-obvious (expression of meibomian glands needed to view quality and quantity of meibum).5 Acne rosacea causes MGD 50 % of the time. The Tear Film & Ocular Surface Society (TFOS) International Panel on MGD discussed how MGD is progressive and pathophysiology leads to loss of oil, tear film barrier, and eventual meibomian gland atrophy.6 In a recent study by Lemp et al., 79 % of patients with dry eye had MGD alone, 23 % had aqueous deficiency alone, and 57 % had a combination of both MGD and aqueous deficiency, suggesting that evaporative dry eye is the most common cause of dry eye seen in 86 % of patients.7
Aqueous deficiency is typically most common in postmenopausal women over age 50, approaching approximately 12 million individuals in the US. Other risk factors for this category of DED includes prior corneal refractive surgery, autoimmune diseases (diabetes mellitus, thyroid disease, rheumatoid arthritis, lupus, mixed connective tissue disease, fibromyalgia, Sjogren’s syndrome), patients with low blink rate such as computer vision syndrome and Parkinson’s disease, prior eyelid surgery, such as ptosis repair and blepharoplasty, and contact lens users. Medications such as antihistamines, diuretics, beta blockers, tricyclic antidepressants, anxiolytics, antispasmodics, hormone replacement therapy, and birth control pills are among the many that can contribute to dry eye and aqueous deficiency. With the new DEWS definition, the tear film in aqueous deficiency typically has elevated electrolytes measurable as osmolarity, decrease in protective enzymes and antibodies, and elevation in inflammatory cytokines.
Ocular allergy completes the triad that can affect the ocular surface. Patients may have perennial allergies caused by dust mites and/or animal dander or may have seasonal allergies caused by tree, grass, and/or ragweed pollens. All forms of allergy treatment (topical, intranasal, inhaled aerosols, and/or systemic) will typically cause dry eye and/or dry mouth as a side effect of treatment, complicating an already complex ocular surface.8–10
Diagnostic Armamentarium for Dry Eye
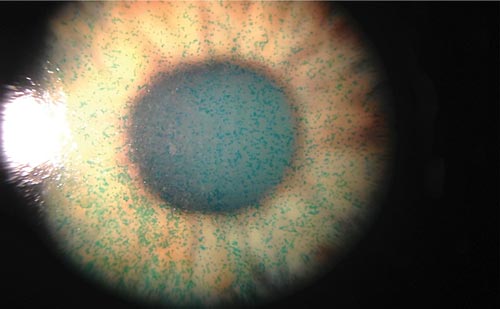
Current clinical measures to evaluate the ocular surface include tear secretion tests such as Schirmer (basic secretion test [BST] with topical anesthesia, or Schirmer I without anesthesia), vital dye staining of the cornea and/or conjunctiva with lissamine green and/or fluorescein, tear breakup time (TBUT), conjunctival impression cytology (goblet cell analysis, quantification of inflammatory markers such as human leukocyte antigen [HLA]-DR), tear osmolarity, tear film thickness of the lipid layer, nonspecific inflammatory markers of the tear film such as metalloproteinase-9 (MMP-9), immune blood titers, and meibomian gland dropout in the tarsus. Quantifying tear osmolarity (Tear Lab) is a reliable method to diagnose aqueous deficiency and monitor a patient’s response to treatment in general. A tear osmolarity greater than 308 mOsm/l in either of the two eyes measured and/or a difference of greater than 8 mOsm/l between the two eyes is a hallmark of tear film instability.11–13 No different from a diabetic measure of glycated hemoglobin (HbA1C) as a measure of blood sugar control, tear osmolarity is a good measure of dry eye severity and therapeutic response. Research has even shown high osmolarity to be associated with an increase in MMP-9 and a loss of epithelial cell–cell junctions.14 Recent literature has even demonstrated that tear osmolarity is the best predictor of disease severity compared with Schirmers, TBUT, meibomian gland scoring, Ocular Surface Disease Index (OSDI) questionnaire, and corneal/conjunctival staining.12 Another in-office quick diagnostic test is measurement of the nonspecific inflammatory marker MMP-9 (InflammaDry®, RPS), where a positive result detects levels greater than or equal to 40 ng/ml in the tear film.15,16 Other research shows statistically elevated levels of MMP-9 activity in tear samples in both patients with MGD and Sjogren’s syndrome, the latter typical of aqueous deficiency.17
Sjogren’s syndrome is a chronic, systemic, progressive autoimmune disease is undiagnosed in one out of every 10 dry eye patients. It is characterized by an immune-mediated lymphocytic destruction of the lacrimal and salivary glands, causing early hallmark symptoms of dry eyes and dry mouth.18 The disease can present alone as primary Sjogren’s or related to another autoimmune disease (e.g. rheumatoid arthritis) classified as secondary Sjogren’s. It currently takes 4.7 years to receive an accurate diagnosis with current classic immunological titers anti-Rho/SS-A and anti-La/SS-B antibodies. Delayed diagnosis in these patients can lead to lymphomas, interstitial lung, or kidney disease, as well as many other devastating systemic diseases. Recent identification of additional serologic markers has improved the sensitivity and specificity of Sjogren’s detection at a much earlier stage of the disease. These new titers are salivary protein 1 (SP-1), carbonic anhydrase 6 (CA-6), and parotid secretory protein (PSP), all with high levels of expression in either the lacrimal glands and/or acinar cells of the submandibular, parotid, and salivary glands.19 Confirmatory diagnosis of Sjogren’s syndrome requires at least two of the following three: clinical evidence of dry eye as described in this paper, positive serological titers as described above, and/or dry mouth confirmed by salivary gland biopsy.18
Patient questionnaires such as the Standard Patient Evaluation of Eye Dryness (SPEED) and OSDI are useful fast screening tools for DED in both clinical practice and clinical studies. The SPEED questionnaire specifically evaluates both the frequency and severity of symptoms and is one of the tools used to identify candidates for lipid layer analysis with LipiView (TearScience).20,21 LipiView uses advanced interferometric technology to provide a relative measure of the thickness of the lipid layer of the tear film. It produces a measurement called the ocular index of lipid interferometric color unit (ICU) calculated on a frame-by frame basis and plotted for approximately one billion data points per eye. The ICU levels as a minimum (MIN) ICU, maximum (MAX) ICU, and average (AVG) ICU are displayed on the LipiView report for easy clinician analysis. AVG ICU levels below 100 are suggestive of a poor lipid layer in the tear film. The Meibomian Gland Evaluator ([MGE], TearScience) is also an excellent way to evaluate the secretions from the meibomian gland orifices through a slit lamp biomicroscope in a quantitative and reproducible way due to its consistent moderate pressure between 0.8 g/mm2 and 1.2 g/ mm2.22 Korb et al. showed a statistically significant correlation between the number of meibomian glands that will express liquid using the MGE device and the severity of symptom level patients had for their dry eye concerns by utilizing the SPEED questionnaire in this study.22,23
The International Task Force (ITF) created consensus guidelines in terms of diagnostic signs and symptoms and treatment considerations.4 ITF level 1 reveals conjunctival staining (best seen with lissamine green [LG]), level 2 adds corneal staining and poor TBUT, level 3 adds filamentary corneal findings, and level 4 adds conjunctival scarring. The Dry Eye WorkShop (DEWS) diagnostic template for staining recommends dividing the cornea into five regions and interpalpebral conjunctiva into six regions with a grading scale of 0 to 3 in each region. To simplify the process clinically, it is best at the minimum to grade the central cornea and inferior cornea staining and be consistent with your ITF classification and grading between exams. The central cornea is the hallmark of severe disease and the inferior cornea is the most common location of staining. Staining is maximized on the corneal and/or conjunctival surface if you allow for 60–90 seconds after vital dye instillation. Neither tear osmolarity, MMP-9 activity, nor lipid layer analysis was part of the original ITF diagnostic classification, and all three can be quite beneficial in solidifying a proper dry eye diagnosis leading to better therapeutic decision-making.
Therapeutic Options for Dry Eye
The ITF delineated treatment recommendations based the level of dry eye severity diagnosis. Topical cyclosporine 0.5 % (Restasis®, Allergan) was recommended for level 2 and above with the addition of punctal plugs for level 3 and above. Topical cyclosporine is believed to inhibit T cell activation, recruitment of additional T cells, and reduction in cytokine production in the inflammatory process of dry eye.24,25 Rao et al. in their follow up to his original READY (Restasis vs Endura Assessment of Disease for 1 Year) publication showed continued increased tear production with Restasis use at 2 years compared with control in patients with chronic dry eye due to ocular inflammation.26 Because Restasis can take up to 8 to 12 weeks to have complete therapeutic effect, topical steroid anti-inflammatory eye drops, such as loteprednol etobanate 0.5 % gel, can be used during this induction phase for Restasis. Hypotonic artificial tears have also shown to reduce tear film osmolarity as measured quantitatively based on the new DEWS definition for dry eye.27
The real dilemma with the current ITF treatment recommendations is a lack of guidance for evaporative dry eye and ocular allergy treatment options in the complex ocular surface. Fortunately, the newest topical allergy eye medications are combination agents blocking H1 receptor activity at the corneal nerve level to prevent itching and blocking mast cells from releasing histamine and other inflammatory mediators responsible for chemosis, vasodilation, edema, and hyperemia. The newest topical combination agents on the market that have the highest specificity for the H1 receptor and without the muscarinic side effects of dry eye are bepopastine 1.5 % (Bepreve®, Bausch & Lomb) and alcaftididine 0.25 % (Lastacaft®, Allergan).28–30 Performing allergy skin testing with in-office kits (such as available from Doctor’s Allergy Formula) also helps patients learn to avoid specific allergens seasonally or perennially and utilizing high-efficiency particulate air (HEPA) filters at home and/or dust mite prevention linens if necessary.
Evaporative dry eye can present alone or in conjunction with aqueous deficiency and may need a combination of many therapies. Additional therapeutic options not already discussed may include warm compresses/ goggles,31 lid massage, eyelid cleansing scrub pads/foam, topical eye meds, systemic meds, nutraceuticals, and eyelid devices. Topical eye meds may include topical azithromycin (Azasite®, Akorn), combination antibiotic-steroid such as tobramycin and loteprednol 0.5 % (Zylet®, Bausch & Lomb) or tobramycin/dexamethasone (Tobradex ST®, Alcon), and/or artificial tears that replace the lipid layer such as Retaine MGD™ (OCuSOFT), Systane Balance® (Alcon), Refresh Optive® Advanced (Allergan), Soothe® XP (Bausch & Lomb), or Liposome sprays for those patients that cannot place eye drops in their eyes. Systemic medications, such as low-dose doxycycline at 50 mg/day and/or nutritional supplements with omega fatty acids (FAs) that offer an anti-inflammatory benefit due to high gamma linolenic acid (GLA) content (Eye Relief, Doctor’s Advantage™; HydroEye®, Science-Based Health), can also provide relief for those patients with evaporative dry eye.32 There are three FA candidates for dry eye therapy: GLA is a unique omega-6 not present in the diet and only obtained by supplements from black currant seed oil. Eicosapentaenoic (EPA) is an omega-3 found in coldwater fatty fish and/or fish oil supplements. Alpha-linolenic acid (ALA) is an omega-3 found primarily in flaxseed oil supplements. The HydroEye clinical trial statistically showed the true benefit of GLA supplements in terms of improved OSDI scores, improved corneal smoothness, and lower inflammatory marker levels than placebo.32 Lastly, eyelid procedures such as intraductal meibomian gland probing/expression with devices developed by Steve Maskin (Rhein) or the LipiFlow thermal pulsation (TearScience) as aided by the lipid layer LipiView analysis can be more definitive in the treatment of evaporative dry eye.
LipiFlow Thermal Pulsation System is truly an advanced treatment option for MGD/evaporative dry eye patients and can effectively and safely treat meibomian gland obstruction in both the upper and lower eyelids simultaneously as an in-office procedure, taking only 12 minutes per eye. The LipiFlow system utilizes a sterile disposable eyepiece connected to a digital console used by the clinician to control the application of heat and pressure to the eyelids33 (see Figure 1). The lid warmer resembles a large oval scleral lens designed to rest on the bulbar conjunctiva and vaults the cornea. The concave side to the lid warmer comprises an insulating material that, in addition to the air gap created by the corneal vault, shields the cornea and ocular surface from direct exposure to the heat applied. The convex side of the lens warmer contains an imbedded precision heater to regulate the temperature applied to the inner surface of the eyelids, providing heat to the palpebral surfaces of the upper and lower eyelids directly over the meibomian glands with a nominal average temperature between 41 and 43°C. The activator is composed of an inflatable air bladder, which rests over and compresses the closed eyelids providing graded pulsatile pressure to the outer eyelid. The LipiFlow treatment only requires 1 to 2 drops of topical anesthetic to the treatment eye. Patients with obstructed meibomian glands achieve the best results with this treatment, and glands with atrophy will have little response with LipiFlow.
LipiFlow received US Food and Drug Administration (FDA) approval based on its open-label, randomized, controlled, multicenter trial compared with warm compress therapy for the treatment of MGD.34 Selected inclusion criteria was a minimum age of 18 years, history of dry eye symptoms within 3 months of the baseline examination, SPEED score of ≥6 at the baseline visit (range 0–28, with ≤5 score as typically asymptomatic), and meibomian gland secretion score of ≥12 for 15 glands of the lower eyelid evaluated with the MGE device. Two hundred and seventy-eight eyes in 139 patients at nine investigational sites received in a 1:1 treatment randomization either LipiFlow or warm compress therapy with the latter receiving LipiFlow in a crossover treatment 2 weeks later. Both arms were then evaluated at 4 weeks, including 1 day safety evaluation visits after LipiFlow treatment. LipiFlow treatment statistically increased mean meibomian gland secretion score from a mean of 6.3 at baseline to a mean of 16.7 at 4 weeks (see Figure 2). LipiFlow treatment significantly improved mean TBUT from a mean of 5.5 seconds at baseline to a mean of 7.4 seconds at 4 weeks (see Figure 3). Lastly, LipiFlow statistically decreased the frequency and severity of dry eye symptoms based on SPEED score questionnaire post treatment (see Figure 4). There was similar improvement in effectiveness trends observed after crossover from warm compress therapy to LipiFlow treatment as well. In terms of safety, there were no unanticipated or serious device-related adverse events reported with LipiFlow. There was no ocular allergy flareups related to the treatment either as this was a localized heat therapy to the meibomian glands and not to the entire ocular surface. There was no difference in mean change in intraocular pressure (IOP) of logMAR best spectacle-corrected visual acuity (BSCVA) from baseline to after treatment in the LipiFlow versus control group. On a 0 to 10 comfort scale, mean (± standard deviation [SD]) patient discomfort score was 1.4±1.4 during LipiFlow and 0.2±0.6 immediately after treatment. In the study, as directed in the device labeling, two drops of topical anesthetic (e.g., proparacaine or tetracaine) were instilled prior to device insertion. This was to facilitate insertion by reducing the sensation on the eye (cornea/conjunctiva). However, the discomfort during the LipiFlow procedure is primarily from the pressure application to the eyelid, and these topical anesthetic drops do very little to anesthetize the pressure feeling to the eyelid. In addition, the effects of these drops begin to wear off prior to completion of the 12-minute procedure. Based on a published study, the anesthesia from 1 drop of proparacaine lasts 10.7 minutes and 1 drop of tetracaine lasts 9.4 minutes.35 Therefore, the anesthetic effects on the eye sensation are likely reduced by the end of the LipiFlow procedure (approximately 15 minutes after instillation assuming 3 minutes of prep time prior to initiation of device treatment). The LipiFlow System per FDA labeling is intended for the application of localized heat and pressure therapy in adult patients with chronic cystic conditions of the eyelids, including MGD, also known as evaporative dry eye or lipid deficiency dry eye.
In summary, the ocular surface is really a complex array of environmental influences, MGD, and inflammatory mediators. Deciphering if the patient has an evaporative dry eye, aqueous deficient dry eye, or both with or without an additional ocular allergy insult is important in paving the way to a proper treatment regimen as described by both the DEWS report and TFOS panel on MGD. LipiFlow Thermal Pulsation System based on its FDA approval is the first to actually treat the cause of evaporative dry eye in a clinically significant way with the aid of LipiView lipid layer analysis and other advanced diagnostic markers discussed. Since its FDA approval, there have many independent results match-sponsored trials to support the use of LipiFlow for evaporative dry eye.36,37