Infections, inflammation and trauma to the cornea and ocular surface can culminate in loss of corneal transparency and subsequent compromise of visual function. This can have significant associated physical and psychological morbidity, as well as a profound socioeconomic impact.1,2 The major causes of corneal inflammation and scarring include microbial keratitis,3 chemical and thermal injuries,4,5 persistent epithelial defect6 and corneal stromal melting,7 as well as iatrogenic causes such as surgery and photorefractive keratectomy.8
The corneal wound healing response is a complex cascade of cytokine- and growth-factor-orchestrated interactions between epithelial and stromal cells, corneal nerves, the tear film and the cells f the immune system. Irrespective of the type or extent of injury, the response is generic: upon wounding, whether it is simply an epithelial abrasion or a compound chemical injury involving both the epithelium and the stroma, induction of the apoptotic cascade occurs, leading to the loss of keratocytes adjacent to the site of injury. There is also activation, proliferation and differentiation of keratocytes into fibroblasts, resulting in repair and remodelling of the corneal stroma. In addition, the surface epithelium undergoes migration and proliferation. Simultaneously, the basal epithelium will migrate and proliferate across the area of epithelial loss as a monolayer of cells. Following complete coverage of the denuded area, there is stratification of the monolayer, resulting in complete anatomical restoration of the epithelium. Cell–stroma adhesion complexes begin to form, but may take weeks or months to stabilise. In the evolutionary context, the healing of the ocular surface must be rapid as vision is essential for the survival of most animals, hence initial corneal epithelial healing occurs quickly. Upon completion of epithelial healing, and depending on the degree of stromal damage, fibroblasts begin to revert to their inactivated state. However, this process may take months, as reflected in the stromal haze that is often seen following excimer photorefractive keratectomy.9
Although epithelial healing is rapid in most cases, under certain conditions epithelial healing can be delayed or impaired, resulting in persistent epithelial defects. Such conditions include chemical and thermal injury, severe keratoconjunctivitis sicca, limbal stem cell deficiency and cicatrising conditions such as Stevens-Johnson syndrome and ocular cicatricial pemphigoid. These conditions can be very challenging to treat and may require prolonged hospital admission and intensive instillation of topical medication.10,11
Current Modes of Drug Delivery for Corneal Wound Healing
Over 90% of ophthalmic treatments are in the form of topically administered eye drops. This mode of drug delivery is utilised to treat both the ocular surface and conditions requiring the intraocular penetration of medication. Although eye drops are a convenient and non-invasive modality of drug delivery, several drawbacks exist, including limited drug reservoir in the conjunctival sacs, leading to loss of the medication. This is compounded by rapid tear turnover, nasolacrimal drainage and rapid evaporation from the pre-ocular surface. As less than 5% of the applied medication reaches the intraocular tissues, the requirement for more frequent instillation of topical medication inevitably leads to increased systemic absorption of the drug, thereby increasing the risk of systemic side effects.12 This has necessitated the development of alternative modes of drug delivery that maximise ocular drug bioavailability and minimise systemic absorption by reducing the need for frequent topical drug administration. These new modes of drug delivery include nano- and microparticles, liposomes, collagen shields and hydrogels,12 all of which have been shown to be successful in prolonging drug release. Although collagen shields are commercially available and have been successfully used in the administration of drugs to the ocular surface, there are reservations regarding their use due to their bovine or porcine origins.13
An additional treatment modality is the use of amniotic membrane, which has a growing role in the management of many ocular surface conditions. In particular, it has a distinct role in the adjuvant management of chemical and thermal burns and persistent epithelial defects, as well as acting as a carrier for ex vivo expanded corneal epithelial cells for use in ocular surface reconstruction. The amniotic membrane is believed to promote wound healing, reduce scarring, aid epithelialisation and reduce pain. It also possesses antiangiogenic and antimicrobial properties (for a review see Dua et al.10). Amniotic membrane consists of an epithelium, an associated basement membrane and a thick stroma layer; clinically, it can be used as a patch or a graft. When applied basement-membrane-side-down on the ocular surface to act as a biological bandage, it is described as a patch. The aim of such a patch is to protect the ocular surface and promote epithelialisation, but, ultimately, it never becomes incorporated onto the ocular surface. When utilised as a graft, the amniotic membrane is applied stromal-side-down and basementmembrane- side-up. Here, the amniotic membrane is acting as a substitute basement membrane to permit host epithelial cell migration; thus, it is envisaged that the membrane will become incorporated onto the ocular surface.10,11
Although many reports have described the successful use of amniotic membrane in ocular surface reconstruction, there have also been several documented cases of sub-optimal results.11,14 As such, further investigations of the structural and biochemical properties have revealed significant intra- and inter-donor variations, which may account for the failures that have been reported. Moreover, there is significant variation in the procurement and subsequent preparation of the amniotic membrane for surgery, thus the membrane is less than standardised.15 These problems are further compounded by the fact that the amniotic membrane, being a biological tissue, must be screened for transmissible diseases and be quarantined prior to clinical use. Nevertheless, transmission of micro-organisms may still be a significant risk.10,11,15 These shortfalls have led researchers to consider synthetic alternatives that can be used as readily available standardised alternatives to the native amniotic membrane. As such, hydrogel polymers have frequently been exploited: not only can they be used to act as scaffolds to support cell migration and growth, but also they can act as drug delivery vehicles for the release of medications, growth factors and/or cytokines.
Hydrogels in Ophthalmology
Hydrogels are hydrophilic polymeric networks that are capable of imbibing large quantities of fluid. They exist in a liquid state (sol), but can be induced to convert to a semi-solid state (gel) by various chemical or physical cross-linking methods.16 Since their original introduction as soft contact lenses in the 1960s,17 hydrogel polymers have gained increasing popularity in many biomedical applications.16,18–21 As such, there is a vast diversity of hydrogels being used and studied in the biomedical field. Corneal wounds secondary to trauma and surgery are currently secured with nylon sutures, which are left in situ or removed at a later date. This extra surgical step has warranted the development of hydrogel adhesives – highly branched biocompatible dendrimer polymers that exhibit high tensile strength and that can be utilised to secure corneal wounds. These polymers consist of a central core component upon which additional generations of monomers are coupled in a divergent manner. Research has focused mainly on the synthesis and characterisation of biocompatible polyesters, polyester–ether and polyamide dendrimers. These polymers are frequently cross-linked and polymerised using an argon ion laser (i.e. they are not thermosensitive) and, although they have demonstrated some promising results, they remain at the experimental stage and have yet to reach clinical practice or applications.22
Thermosensitive Hydrogel Polymers
Stimuli-responsive hydrogel polymers can be induced to switch from a liquid to a stable gel by changes in pH, ionic strength, light and/or temperature. Thermosensitive hydrogels are of particular interest in biomedical applications due to the fact that they remain in the liquid (sol) state outside the body but, on injection or application to part of the human body, the increase in temperature results in formation of a gel that is in direct contact with the desired body cavity or surface. These gels can also potentially be exploited as synthetic scaffolds for tissue regeneration, as well as acting as a mode of controlled delivery for a variety of therapeutic agents.19,20,23,24 As many thermosensitive hydrogel systems are currently in existence, it is beyond the scope of this article to highlight all of them (for a review see Ruel-Gariepy et al.24). Poloxamer (Pluronic®) hydrogel polymers comprise more than 30 non-ionic surface-active agents with a varying range of molecular weights. They consist of varying ratios of polyethylene oxide–copropylene oxide–co-polyethylene oxide (PEO–PPO–PEO), and are often referred to as ABA-type co-polymers. They have been shown to be successful drug delivery systems. The gelation mechanism of these poloxamers has been extensively investigated and is believed to form as a result of thermo-induced changes in micellar properties.16 Timolol maleate has been successfully incorporated into this system and has resulted in a formulation that enhances the ocular bioavailability of the drug.21,25 Mitomycin C has also been successfully incorporated into a thermosensitive gel consisting of methylcellulose and poly(ethylene glycol) (PEG) for subconjunctival application to modulate wound healing following trabeculectomy. This delivery system has been shown to provide better contact with the sclera and conjunctiva at the desired location.26 Although potentially effective as a drug delivery vehicle, poloxamers are mechanically weak, undergo rapid dissolution and are non-biodegradable.25,27 Thus, such materials would not be suitable to act as scaffold supports for tissue regeneration. Nevertheless, the poloxamers remain a viable mode of drug delivery that may be utilised for the modulation of ocular surface inflammation and wound healing.
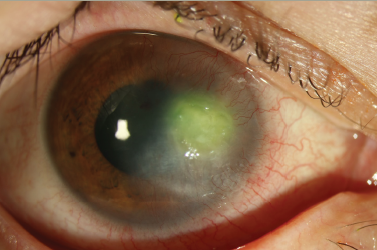
More recently, a synthetic thermosensitive hydrogel has been developed that can be used as a drug delivery carrier, as well as acting as a scaffold for cellular growth on the ocular surface.28 This polymer blend is often referred to as a ‘triblock’ and consists of poly(DL-lactideco- glycolide) (PLGA) and PEG in varied ratios. This PLGA–PEG–PLGA triblock co-polymer is a water-soluble, biodegradable hydrogel that has been proposed for use in the delivery of various therapeutic agents.23,28,29 Furthermore, it has been demonstrated that by varying the concentration of the polymer, the onset and strength of sol–gel transition can be altered for use in specific applications. At a 35%w/v concentration, the desired profile of gelation temperature and gel strength was achieved for applications in ophthalmology28,30 (see Figure 1). The examination of the ultrastructure of the hydrogel using cryoscanning electron microscopy revealed a porous network with the potential to permit cells to utilise the polymer as a scaffold for migration and growth.28 Interestingly, in its unmodified form the polymer is inert and does not allow cellular adhesion. However, additional modification by the introduction of synthetic adhesion peptides should allow the proliferation, migration and differentiation of cells to occur.31 This can be further augmented by the addition or entrapment of growth factors and cytokines in the hydrogel. This PLGA–PEG–PLGA triblock has been shown to be biocompatible in vitro and in vivo in animal models. The unmodified polymer applied to keratectomy and intralamellar wounds of rabbits (see Figure 2) did not hinder reepithelialisation compared with negative controls. Subsequent histological analysis of the cornea showed minimal scar tissue with normal keratocyte appearance; importantly, there was no evidence of an immune response.28 In addition to being a biocompatible and biodegradable scaffold for tissue engineering applications, it has been shown that the PLGA–PEG–PLGA triblock may also be exploited as a drug delivery vehicle, allowing the incorporation of model proteins and their subsequent localised controlled release. Moreover, it has been demonstrated that by varying the polymer blend composition and ratio, specific release profiles of multiple drugs and/or growth factors may also be obtained.30 Such a mechanism may be greatly beneficial to ophthalmological applications in which a cascade of biological response or the delivery of several drugs with independent release kinetics is required.
Conclusions and Future Directions
Hydrogel polymers are a heterogeneous group of polymers that have immense potential for biomedical applications. Hydrogels – in particular thermosensitive hydrogels – have been utilised extensively in the minimally invasive administration of drugs into body cavities and biological surfaces. In relation to ophthalmic use, thermosensitive hydrogels have been extensively investigated as a mode of prolonged drug delivery to the ocular surface. However, in the role of ocular surface tissue regeneration, research and literature is scarce. Recent publications have given insight into the use of the PLGA–PEG–PLGA triblock thermosensitive polymer in ocular surface tissue regeneration and advanced drug delivery. It has been shown to be a biocompatible and biodegradable scaffold with immense potential in ocular surface regeneration. However, there is no doubt that extensive research is required to investigate such new polymers and strategies that can be employed for ocular surface reconstruction and regeneration.