Keratoconus (KC) is a non-inflammatory corneal ectasia; it’s bilateral in up to 90 % of patients and usually asymmetric, unilateral cases occur. However, it has been shown1 that when diagnostic criteria and computer-assisted topographical analysis allow the detection of very early keratoconus in the fellow eye the incidence of unilateral involvement is probably in the range of 2–4 %. There is no sex or race predilection.2 Its presentation is usually sporadic and isolated, although a positive family history can be found in up to 10 % of cases. Reported estimates of the prevalence of keratoconus vary widely, because of the variation in diagnostic criteria. Most estimates fall between 50 and 230 per 100,000.3 The onset of keratoconus occurs at about the age of puberty. The cornea begins to thin and protrude, resulting in irregular astigmatism. Typically, over a period of 10 to 20 years, the process continues until the progression gradually stops.
The optical management of keratoconus is with spectacles or soft contact lenses at initial stages. But when the disease progresses, corneal distortion and irregular astigmatism become higher and the correction must be made using rigid gas permeable contact lenses to provide a regular refractive surface, thus improving visual acuity.4 Laser in situ keratomileusis (LASIK) and other corneal laser refractive surgeries are contraindicated in keratoconus patients as it may worsen the disease by further thinning the cornea.5 Intracorneal rings can regulate the cornea, reducing irregular astigmatism, but some spherical refractive error may remain uncorrected.6 Crosslinking is indicated in cases of keratoconus progression to improve the biomechanical strength and stops its progression. The use of phakic anterior chamber intraocular lenses (pIOL) to treat refractive errors associated with keratoconus has shown to be an effective procedure in cases where the keratoconus is stable. In advanced stages, a keratoplasty technique may be necessary to restore the vision.
Iris Claw Lenses
The iris-claw IOL was used for the first time in aphakic eyes after intracapsular cataract extraction. In the year 1953, the first-generation models, such as the Binkhorst7,8 and the Medallion IOLs,9 were associated with complications such as cystoid macular oedema, corneal decompensation, lens dislocation, uveitis and glaucoma.10 In 1978, Worst designed the iris-claw or ‘lobster claw’ IOL, a coplanar single-piece poly(methyl methacrylate) (PMMA) IOL that was enclavated in a fold of mid-peripheral iris stroma, a relatively immobile portion of the iris. Many surgeons have used the iris-claw IOL after intracapsular cataract extraction or as secondary implantation in aphakia. In 1986, Fechner and Worst implanted the IOL in the first sighted myopic phakic eye with good predictability in the follow up.11
Poly(methyl methacrylate) Iris-Claw Anterior Chamber Phakic Intraocular Lenses
The iris-claw Artisan (Ophtec BV)/Verisyse (Abbott Medical Optics, Inc) is a single-piece non-foldable IOL made of Perspex CQ-UV, a UV light–filtering PMMA material. It is available for the correction of myopia, hyperopia and astigmatism, as well as for aphakia.
The optic vaults approximately 0.87 mm anterior to the iris, which provides good clearance from both the anterior lens capsule and the corneal endothelium. The distance from the optic edge to the endothelium ranges from 1.5 to 2.0 mm depending on the dioptric power, anterior chamber anatomy and optic diameter.
Two models to correct myopia are currently available: Model 206 has a 5.0 mm optic with power ranging from -3.0 to -23.5 D in 0.5 D increments. Model 204 has a 6.0 mm optic and is consequently limited to a smaller range of powers because of its greater proximity to the endothelium in the periphery of the IOL; the power ranges from -3.0 to -15.5 D in 0.5 D increments. For the correction of hyperopia, model 203 incorporates a 5.0 mm optic with power ranking from +1.0 to +12.0 D in 0.5 D increments. Myopic pIOLs have thicker peripheral edges and therefore require more clearance than hyperopic pIOLs. The thickest part of the hyperopic IOL is central, where the anterior chamber depth (ACD) is greater. The toric model has a 5.0 mm optic and is available in powers ranging from +14.0 to -23.0 D in 0.5 D increments, with additional cylinder from 1.0 to 7.0 D (plus or minus cylinder) in 0.5 D increments and oriented at 0 degree or at 90 degrees.
The phakic Artisan/Verisyse has a fixed overall length of 8.5 mm (7.5 mm for paediatric implantations or small eyes), which is a great advantage to the surgeon because he/she does not have to deal with sizing measurements. Another major advantage of these pIOLs is that they can be properly centred over the pupil, even when the pupil is off centre, a relatively common situation among people with high ametropia. Moreover, the fixation system inhibits IOL movement,12 which warrants the correction of astigmatism and may help to correct other vectorial or asymmetrical aberrations in the future.
Foldable Iris-Claw Anterior Chamber Phakic Intraocular Lens
The foldable version of the Iris-Claw Anterior Chamber pIOL is the Artiflex (Ophtec B.V., Groningen, The Netherlands) and Veriflex (AMO Santa Ana, CA). They are made of a hydrophobic polysiloxane. The Artiflex and Veriflex has advantages over the Artisan and Verisyse IOLs as it can be inserted through a smaller incision (3.1 mm versus 5.2 or 6.2 mm) and the distance between the endothelium and periphery of the IOL optic is independent of the dioptric power. Optic design is 6.0 mm and power ranging from -2.0 to -14.5 D in 0.5 D steps. The toric model of the Artiflex is also available in Europe and corrects cylinder from -1 to -5 diopters.
Selection Criteria
Anatomical requirements:
- ACD measured from the endothelium: ≥2.8 mm;
- endothelial cell count (ECC) >2,300 cells/mm2: (>2,500 cells/mm2 if >21 years old, >2,000 if >40 years old). Although this limitation is not valid in post-keratoplasty eyes, were the decision will rely on the surgeon’s opinion;
- irido-corneal angle ≥30°;
- no anomaly of iris or pupil function;
- mesopic pupil size <5.0–6.0 mm; and
- stable topography and refraction at least one year.
Phakic IOLs are contraindicated in:
- Unstable keratoconus or refraction;
- background of active disease in the anterior segment;
- recurrent or chronic uveitis;
- any form of clinically significant cataract; and
- IOP >21 mmHg or glaucoma.
Surgical Technique
Intraocular Lens Power Calculation
The most commonly used method to calculate pIOL power is the van der Heijde13 and Fechner et al.14 formulas, which include the patient’s refraction, keratometry and adjusted ultrasound central ACD. The measurements are independent of the axial length. Moreover, the position in the anterior chamber defines the distance between the pIOL and the retina. Based on this formula, the manufacturers provide nomograms or software to calculate the required power. The one-size-fits-all overall diameter of 8.5 mm prevents complications due to sizing errors that may occur with angle-supported or sulcus-supported pIOLs.
Poly(methyl methacrylate) Iris-Claw Toric Phakic Intraocular Lens
Depending on the surgeon’s familiarity with the technique, general, retrobulbar, peribulbar, or topical anaesthesia can be used. For the Verisyse pIOL implantation procedure, retrobulbar or peribulbar anaesthesia is generally recommended. According to our recommended technique, a two-plane, 5.2 or 6.2 mm posterior corneal incision is centred at 12 o’clock and two vertical paracentesis directed toward the enclavation area are performed at 2 o’clock and 10 o’clock. This incision can be located in other position depending on the axis of the cylinder to be corrected. Alternatively, a scleral incision can be used. Wound construction is important to minimise induced astigmatism or wound leaks. Some surgeons locate the incision on the steep corneal meridian.
The pupil should be constricted to protect the crystalline lens from contact with the pIOL or the instruments during surgery. This can be achieved by instilling pilocarpine 1.0 % preoperatively or injecting acetylcholine (Myochol) in the anterior chamber at the beginning of the procedure. Taking advantage of the capability to locate this type of pIOL over the centre of the pupil, the centre should be marked preoperatively if using pilocarpine 1.0 % or at the beginning of surgery if using intracameral acetylcholine to enable proper centration of the pIOL and to mark the precise axis for the toric implantation. After the anterior chamber is filled with a cohesive OVD, the IOL is introduced and rotated 90 degrees into a horizontal position or in the axis previously marked when implanting the toric version. The pIOL is fixated with an enclavation needle that has a bent shaft and a bent tip that pushes the iris into both claws. The needle is introduced through one paracentesis and holds the fold of iris while the pIOL is slightly depressed with the implantation forceps so the claws will automatically grasp the iris, also recently in the market is the vacufix which comprises two holders with an aspiration tip that can be attached to the phaco machine. A vacuum is created to clip a precise and replicable amount of iris tissue between the haptics of the lenses. The advantages of this technique are precision for the patient and surgeon, speed and convenience and, accordingly, comfort for the patient and can be used in both rigid and flexible type of the pIOL. Hands are then switched and the same manoeuvre is performed through the other paracentesis. Both fixation of the iris claws and proper centration of the pIOL over the pupil should be checked before the next step, which is one of the main advantages of this pIOL style. At the end of surgery, it is not unusual to have mild ovalisation of the pupil due to the effect of the miotic agent. If the pIOL is not well centred, enclavation can be released by pushing in the central portion of the claw with the enclavation needle.
A peripheral iridectomy should be performed to prevent pupillary block. Alternatively, a neodymium-doped yttrium aluminium garnet (Nd:YAG) laser can be used preoperatively to create one or two small iridotomies. The corneal wound is then sutured with five interrupted 10-0 nylon sutures and the scleral incision with one running (cross or mattress) suture. Proper tension of the sutures is checked with a standard qualitative Maloney keratoscope. Then sutures are selectively removed, depending on the patient’s refractive and topographic astigmatism, beginning at week four and over a period of three months.
Foldable Iris-Claw Toric Phakic Intraocular Lens
Implantation of the foldable model requires a 3.1 mm incision, which corresponds to the width of the PMMA haptics. The Artiflex/Veriflex pIOL is inserted using a specially designed spatula. The enclavation process is the same as for the PMMA pIOL except that the pIOL is grasped with the implantation forceps at the base of the haptic instead of at the edge of the optic. In order to achieve the precise location in cases of toric implantation, preoperative determination and marking of the cylinder axis is essential. The incision is usually watertight, but some surgeons may prefer a 10-0 nylon suture.
Case Presentation
Artiflex Toric Lens
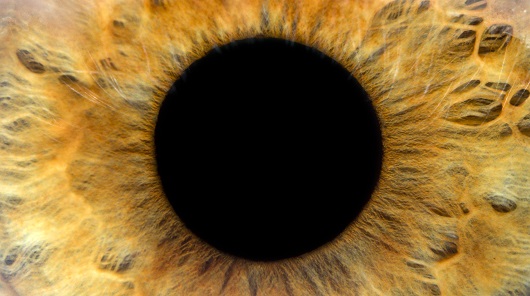
Twenty-eight-year-old female patient who visited us interested in refractive surgery with no history of contact lens wear. Her best-corrected visual acuity (BCVA) in her right eye was 20/20 with -4.50 – 2.00 x 170° and left eye 20/20 with -4.50 – 1.00 x 180°. Topography shows a form fruste keratoconus (see Figure 1). After discussing the options with the patient and explaining the contraindication of a laser corneal procedure, the choice was made to proceed with Artiflex/Veriflex toric iris claw lens implantation (see Figure 2). The endothelial cell count (ECD) was 2,850/2,765 cells/mm2 in right and left eye respectively. Postoperatively, the patient was managed with a combination of antibiotic anti-inflammatory drops four times a day and hypotensive drops two times a day for three weeks and ciclopejic in the night for the first three nights.
Artisan Toric Lens
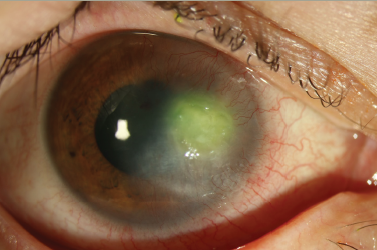
A 52-year-old white man with keratoconus had contact lens intolerance in his right eye. The refraction and keratometry values in the right eye had been stable. The UCVA in the right eye was counting fingers at 2 feet, and the manifest refraction was -11.75–5.00 x 130° with a BSCVA of 20/30. Orbscan topography showed a keratoconic pattern (see Figure 3), ACD was 3.1 mm, scotopic pupil size was 4.2 mm, and ECD was 2519 cells/mm2 with a hexagonality of 31 %. Other than a keratoconic cornea with absent scarring, slit lamp examination of the anterior and posterior segments was within normal limits. An Artisan/Verisyse pIOL (6.0 mm optic) was implanted in the right eye (see Figure 4) in the same manner as described above and a similar post-operative medication regimen as the previous patient but without the indication of cicloplejic.
Conclusion
The use of spectacles to correct ametropias involves minimal risk, though the visual quality achieved in keratoconic eyes is generally deficient, as aberrations, minification and limitation of the visual field are often produced. Apart from that, functional and aesthetic drawbacks may also be present. Contact lenses give users greater visual acuity and quality of vision.15 Even though the availability of highly oxygen-permeable contact lenses has increased the tolerance and safety of extended contact lens wear, their use may be associated with potentially serious complications, especially among chronic users, which may lead to severe vision loss.16–18
Implantation of toric iris-claw Artisan/Verisyse or Artiflex/Veriflex PIOLs offers a good alternative to spectacles and contact lenses, especially for patients with stable keratoconus under 50 years who have not lost accommodation, provided they meet the anatomical requirements outlined in ‘Selection criteria.’ Implantation of iris claw phakic lenses has proved to be effective, stable and very safe.19–28 Keratoconus has been reported to stabilise in the third and fourth decade of life.2 In patients of this age, there is less concern of rapid disease progression and pIOL implantation may have a more lasting effect. In addition, pupil size tends to decrease with age,29 which may be beneficial for iris claw lens centration as well as minimising glare and halo symptoms.22,24
It is important to take into account that many keratoconic patients rub their eyes and need to be reminded that eye rubbing can cause traumatic dislocation of the IOL and accelerated endothelial cell loss. As with penetrating keratoplasty (PKP), the complications of which include allograft rejection, astigmatism, keratitis and glaucoma,30–32 implantation of an iris claw lens certainly involves risks, but normally the keratoconic eyes has deep anterior chambers which made the implantation safers. However, in the event of failure, its removal could leave PKP as a remaining option. For that reason, pIOLs may provide an alternative treatment between rigid gas permeable contact lens (RGP) and PKP.
Nevertheless, the potential risks of these implantations should be borne in mind, especially the loss of corneal endothelial cells. Several studies have examined changes in ECC after implantation of the Verisyse/Artisan and Veriflex/Artiflex phakic IOL. Although some of them have found a significant decrease of endothelial cell density,33,34 data from the European multicentre study of the Artisan PIOL22 and the US Food and Drug Administration (FDA) Ophtec study35 show that implantation of the Artisan iris-claw PIOL did not result in a significant loss of endothelial cell density at up to two years postoperatively.
Regarding intrastromal corneal ring segment (ICRS) implantation in eyes with keratoconus, it has been shown to improve visual outcomes and decrease manifest refraction by strengthening and reshaping the cornea, the range of correction often is limited, the predictability is relatively low and it is not clear if the ICRS can limit the progression of keratoconus. In addition, significant levels of refractive error remain uncorrected in eyes with high ametropia; toric pIOL implantation can also be attempted in such cases.36,37
In cases of unstable or documented progression of the keratoconus corneal collagen cross-linking (CXL) is a good option. It uses a photosensitiser, riboflavin, and UVA light that has been shown to result in increased stiffness of the cornea, improved biomechanical strength, keratocyte apoptosis, and increased resistance to enzymatic digestion.38–41 As a result of these effects, the procedure has been used to limit the progression of keratoconus. After the stability is achieved and documented, a toric phakic iris claw lens can be implanted to correct the residual refractive error.42 With the same concept in mind, they can also be implanted after deep anterior keratoplasty or PKP to correct the residual refractive error once it is stable, this procedure being one of the most common to correct this group of patients who use phackic toric intraocular lenses to correct ametropias post DALK or PKP. ■