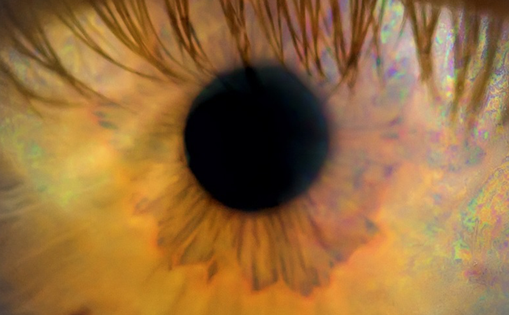
Intraocular viral infections have various presentations. They may be detected as anterior uveitis, intermediate uveitis, acute retinal necrosis (ARN), progressive outer retinal necrosis (PORN) and neuroretinitis (see Figure 1).1,2
Anterior uveitis (AU) in most patients is either idiopathic or associated with HLA-B27 positivity. However, a viral cause of AU is often underestimated. The most common viruses in the aetiology of viral AU (VAU) are herpes simplex virus (HSV), varicella-zoster virus (VZV), cytomegalovirus (CMV) and rubella virus (RV).1–3
Intraocular viral infections have various presentations. They may be detected as anterior uveitis, intermediate uveitis, acute retinal necrosis (ARN), progressive outer retinal necrosis (PORN) and neuroretinitis (see Figure 1).1,2
Anterior uveitis (AU) in most patients is either idiopathic or associated with HLA-B27 positivity. However, a viral cause of AU is often underestimated. The most common viruses in the aetiology of viral AU (VAU) are herpes simplex virus (HSV), varicella-zoster virus (VZV), cytomegalovirus (CMV) and rubella virus (RV).1–3
Recently, the aetiology of some ‘idiopathic’ AU syndromes are proved to be viral. RV and CMV, for example, cause a distinct clinical spectrum of ocular symptoms presenting as Fuch’s Uveitis syndrome (FUS) which strongly suggest that they might be involved in the pathogenesis of FUS.4,5 Interestingly, CMV may also be involved in the pathogenesis of Posner-Schlossman syndrome (PSS).4,6
Diagnosis of VAU depends mostly on clinical findings. The clinical features commonly described in association with VAU include diffuse, fine, stellate or dendritiform keratic precipitates, ocular hypertension and iris atrophy.4,5,7–14 Although clinical features of different VAUs overlap, there are some characteristic findings depending on the causative viral agent.
In this review, the clinical features of the most common VAUs (HSV, VZV, CMV and RV) are presented.
Herpes Viridae Family (Herpes Simplex Virus, Varicella-zoster Virus, Cytomegalovirus)
These DNA viruses are ubiquitous and following primary infection, lifelong latency is a characteristic feature. The three main viruses responsible for ocular inflammation are HSV-1, VZV and CMV. Epstein-Barr virus (EBV) and HSV-2 have also infrequently been detected in ocular disease.15
The worldwide seroconversion to herpes viruses ranges from 60 to 90 %.16–21 VAU, due to either HSV or VZV is reported to be 5 to 10 % of all uveitis cases.22,23 However, other viruses such as CMV and RV are also increasingly being implicated as causative factors, particularly in patients presenting with hypertensive AU.4,5,7–11
Interestingly, the clinical features of herpetic ocular infection depend to a certain extent on the immune status of the patient. CMV infection, for example, predominantly manifests as retinitis in immunocompromised patients.24,25 In contrast, it almost always occurs as AU in otherwise healthy immunocompetent patients.24,25 Similarly, in VZV infection, posterior segment involvement is more likely to occur in immunocompromised patients and they are also more likely to develop chronic disease.26
Herpes Simplex Virus and Varicella Zoster Virus
These two herpes viruses share certain common features in their manifestations and treatment. Frequently, uveal inflammation associated with herpes viruses evolves as keratoiritis associated to corneal disease (see Figure 2). However, HSV associated AU may also occur without noticeable keratitis and may therefore be more difficult to diagnose.12
The prevalence of HSV-1 is generally higher than that of HSV-2 and increases in a linear fashion with age. Seroconversion in adults is about 60 to 90 % worldwide.16 Although the prevalence of HSV is high, ocular involvement in HSV-infected patients is relatively uncommon and has been estimated to be about 1 %.27 The prevalence of VZV AU is often relatively low and was reported to account for 10–13 % of all herpetic AU patients.12,14 This assumption might be incorrect since, even in the absence of skin lesions, VZV AU is not uncommon and known as ‘varicella zoster sine herpete’.28 VZV is known to be the aetiological agent of two clinically distinct diseases: varicella (chickenpox) and herpes zoster (shingles).29 While varicella is the primary infection of VZV, zoster is its secondary infection caused by re-activation of VZV from latency.29 Approximately 90 % of children worldwide are VZV seropositive. Thirty per cent of the elderly experience a reactivation of the latent VZV resulting in a herpes zoster infection, of whom about 10 to 25 % develop herpes zoster ophthalmicus (HZO).30,31 The risk of VZV infection in AIDS patients is significantly higher32 and it may be an early sign of HIV infection.33
Herpetic AU may be accompanied by dermatitis, conjunctivitis, keratitis, scleritis, or retinitis.34–38 It is almost always unilateral and patients most frequently complain of blurred vision, eye pain, redness and photophobia.39,40 Herpetic AU usually follows an acute recurrent course.41 Anterior chamber inflammation may be mild or severe and may even produce a hypopyon or hyphaema.40 Keratic precipitates may appear small, large, or stellate and collect frequently at areas of active keratitis.22,40 Posterior synechiae are common.22,40 Many patients also have decreased corneal sensation,12 an acute rise in the intraocular pressure (IOP),12,13,23,34,41,42 and patchy, sectoral (see Figure 3), or even diffuse iris atrophy.23,36,37,43–45 Sectoral iris atrophy, which results from ischaemic necrosis of the stroma, is a frequent diagnostic sign in patients suffering from herpetic AU.45,46
The acute increase in IOP has been attributed to inflammation of the trabecular meshwork.34 This notion is supported by the observation that intraocular pressure typically normalises in response to topical corticosteroid therapy.34,42 Active keratitis or findings of a previous corneal scar are frequently associated with herpetic AU. Dendritic or geographic ulcers, stromal keratitis and endotheliitis are signs of active herpetic keratitis. Dermatomic vesicular rash involving the ophthalmic division of the trigeminal nerve in patients with VZV, and the peri-ocular area in patients with HSV may also help to distinguish herpetic AU.3 However, in patients with isolated anterior chamber involvement, it is often difficult to determine the causative agent without aqueous humor analysis.
VZV ocular involvement after primary varicella infection is uncommon and may present as uveitis, interstitial keratitis, corneal ring infiltrate, or internal ophthalmoplegia.13,47,48 Ophthalmic involvement typically occurs as part of HZO.
As both HSV and VZV can present similar findings, distinguishing between the two viruses may be quite challenging.22 History and clinical examination may help to determine which virus is more likely the causative agent in some patients.22,23 HSV usually affects children and young adults, whereas VZV is more commonly seen in elderly and immunocompromised patients. Skin lesions in HSV patients usually consist of grouped vesicles, whereas in VZV patients they involve a dermatome among the distribution of ophthalmic nerve. The pattern of dendritic keratitis, when present, may also help to differentiate HSV from VZV uveitis. HSV dendrites are usually branching, with well-developed terminal end bulbs that tend to show fluorescein staining in the ulcer base and rose bengal staining at the border. VZV pseudodendrites, in contrast, are usually slightly elevated, broader and polymorphous, with less regular branching, few terminal end bulbs and central rose bengal staining with fluorescein pooling along the edge.49
Treatment for herpetic AU should be primarily directed against the infectious agent. In addition, anti-inflammatory medications such as topical or even systemic corticosteroids are needed. Cycloplegic agents are often indicated to prevent formation of synechiae during the acute stage of intraocular inflammation.50 Topical antiviral agents are usually ineffective in the treatment of AU but may be indicated in patients with herpes simplex keratouveitis to prevent dendritic keratitis during topical corticosteroid treatment.51 Systemic antivirals such as (val)acyclovir, famciclovir, or brimudine are the mainstay of therapy and prevention of recurrences in patients with severe uveitis.52 Table 1 summarises the systemic antiviral therapy in herpetic AU. Initiation of oral antiviral therapy within the first few days after the onset of varicella-zoster is recommended.37 Patients with herpetic uveitis may require prolonged corticosteroid therapy with very gradual tapering.51,52 Systemic corticosteroids may be necessary at times. The oral dosages are acyclovir 400 mg five times daily or valacyclovir 500 mg two times daily for patients with HSV and acyclovir 800 mg five times daily or valacyclovir 1,000 mg three times daily for VZV disease.52 Oral acyclovir, 600 to 800 mg/day, has been shown to diminish the number of recurrences in patients with herpetic AU when given on a long-term basis.53 Oral acyclovir/valacyclovir has been shown to reduce the incidence and severity of ocular complications, including AU, when given for 10 days starting within 72 hours of onset of skin lesions in patients with herpes zoster ophthalmicus.37,54 Topical and oral ocular antihypertensive agents are often necessary to control the ocular hypertension, especially during the first days of treatment.
Cytomegalovirus
CMV is the most common congenital viral infection, with clinical disease occurring among neonates and immunocompromised patients. CMV infection is ubiquitous worldwide. The seroprevalence of CMV was reported to be between 60 to 90 %.17,55–60
CMV retinitis is the most common ophthalmic manifestation of both congenital CMV infection and that occurring in the immunocompromised patient.24,61 Anterior segment involvement in immunocompromised patients is less frequent and usually is mild.61 However, in immunocompetent patients, CMV has been found in association with corneal endotheliitis as well as AU associated with elevated intraocular pressure (IOP).7,8,62–65
CMV AU may present as ‘acute recurrent AU’ associated with ocular hypertension (resembling PSS) or ‘chronic AU’, which may be complicated by glaucoma (resembling FUS).4,24,25,66 In CMV AU, the anterior chamber inflammation is mild and posterior synechiae do not develop.4,24,25 Typically, the posterior segment is uninvolved.4,24,25 The frequency of acute CMV AU is reported to be approximately two times higher than the chronic CMV AU.4,66
Acute recurrent AU (CMV associated PSS) typically presents in middle-aged patients, with unilateral involvement. It is characterised by recurrent episodes of mild iritis, associated with elevated IOP and diffuse epithelial oedema of the cornea and few fine keratic precipitates. The IOP is normal between attacks, and anterior chamber angle is open.66 Iris atrophy may occur and it is either patchy or diffuse, and is present in 15 % of eyes.66 IOP may exceed 50 mmHg during the attacks and 8–23 % of eyes develop glaucomatous optic neuropathy.66
Chronic AU (CMV associated FUS), contrary to rubella-associated FUS, is seen at older ages (mean age of 65)4,66 and occurs mostly in males.4,5,41,66 Interestingly, most reports of CMV FUS refer to Asian patients, whereas FUS in Europe is more closely related to RV. The eye is minimally inflamed and presents with diffuse, fine and stellate keratic precipitates fairly evenly distributed over the endothelium.4,66 Typical signs are corneal endothelial lesions appearing as white, medium-sized, nodular lesions surrounded by a translucent halo, which are significantly associated with chronic CMV uveitis.4,66 The anterior chamber activity in these eyes is mild and in 60 % of eyes, diffuse iris atrophy is present.4,66 Glaucomatous optic neuropathy develops in 36 % and posterior subcapsular cataract in 75 % of eyes.4 Patches of focal endotheliitis may be also observed.4 Vitritis may also be detected.66
Ganciclovir (and its prodrug valganciclovir) is the only currently used therapy in the management of CMV infections.4,25 Various options of ganciclovir application exist including topical and systemic administration. Even intraocular treatment using intravitreal implants or intravitreal injections have been suggested.25 A positive response to ganciclovir therapy was reported in up to 75 % of affected patients, however, recurrences were reported after cessation of treatment in three out of four patients raising the question of preventive measures.25 Chee et al.25 reported that long-term topical ganciclovir application resulted in a lower recurrence rate and less severe adverse effects as compared to systemic ganciclovir or device implantation. Therefore, they suggested topical ganciclovir therapy in CMV AU. In addition to antiviral therapy, topical corticosteroids and/or non-steroidal anti-inflammatory drugs (NSAIDs) may be useful in reducing ocular inflammation. In selected patients with uncontrolled intraocular pressure, glaucoma medications and/or surgery might be still necessary in the management of CMV AU.4,25
Rubella Virus
The RV is the prototypical teratogenic viral agent. It is transmitted via airborne droplets and epidemics were common worldwide before the rubella vaccine became available. Ocular findings of congenital rubella syndrome include chorioretinitis, cataract, corneal clouding, microphthalmia, strabismus and glaucoma.67 Acquired ocular rubella infections usually result in mild self-limiting conjunctivitis (70 %) or keratitis.1 Posterior segment involvement after RV infection is rare, but includes active chorioretinitis with mild AU, pigment epithelial detachment and overlying bullous retinal detachment. It also may present as bilateral severe panuveitis with deep corneal stromal involvement.68
A number of studies have now shown that a high proportion of patients with features characteristic of FUS have antibodies directed against RV. To a lower extent, RV ribonucleic acid (RNA) can be detected in the aqueous humor of the affected eye.9–11,41,69 The association of RV with FUS might be indirectly supported by the observation that the prevalence of FUS in the US has decreased dramatically since the introduction of a universal, population-based rubella vaccination programme.69 The existence of RV-associated AU is further supported by the identification of RV RNA from eyes of patients who developed transient conjunctivitis and uveitis following vaccination with live vaccines,70,71 The occurrence of iris atrophy, iridocyclitis and cataract as late ocular complication of congenital RV infection also supports the RV-associated AU.72–74
Fuch´s uveitis syndrome is an intraocular inflammatory disease that accounts for up to 6.2 % of all uveitis patients.75,76 Its aetiology remained unknown until a few years ago. More recently, evidence has accumulated that infectious agents are related to FUS. Interestingly, in Europe, RV has been identified in almost all patients, whereas in Asia, CMV has been strongly suggested to be involved in the pathogenesis of FUS.4,11,41 FUS occurs in more than 90 % unilaterally. Common clinical manifestations are the presence of a chronic persistent AU, presenting with diffuse, fine, stellate keratic precipitates, diffuse iris atrophy and/or heterochromia (see Figure 4). The absence of synechiae, posterior subcapsular cataract formation, vitritis and sectoral peripheral retinal vascular leakage with disc hyperfluorescence are further characteristics. Despite persistent vitritis as one of the most frequent clinical findings in FUS, a cystoid macular oedema is almost never seen.77 Secondary complications such as glaucoma have been reported in up to 59 % and vitritis in up to 90 % of all patients with FUS.78,79 Patients may remain asymptomatic for years and the diagnosis is often delayed until the visual acuity is affected e.g. due to early cataract progression. The prognosis is favourable in most patients even though the persistent inflammation. Corticosteroids may modulate intraocular inflammation at the anterior segment, but typically fail to resolve it and do not affect vitreous infiltration. Many experts advice to avoid steroids since the risk of cataract progression and secundary glaucoma increases, whereas the benefit of steroid treatment is rather limited.80 Cycloplegia is almost never necessary. Since no specific antiviral treatment is available to modulate the clinical course of RV AU, treatment is reserved to sight threatening complications such as cataract, glaucoma and vitreous opacification.81
Conclusions
The diagnosis of VAU mainly depends on clinical findings. The summary of the demographics, clinical course, ocular findings and laboratory testing that helps to differentiate the causative viral agent is as follows.
Demographics
Patients with rubella-associated AU (mean age 35 ± 12 years) are younger than patients with HSV-associated AU (mean age 43 ± 15 years), who in turn tended to be younger than patients with VZV-associated AU (mean age 53 ± 23 years).41 On the other hand, acute recurrent CMV AU patients (mean age 37 ± 12 years) are younger than the chronic CMV AU patients (mean age 65 years).4
Clinical Course
The disease course is much more frequently chronic in RV-associated AU (96 %) as compared with HSV (39 %), VZV (40 %) and CMV-associated AU (37 %).66
Anterior Chamber Activity
Inflammatory activity in RV and CMV AU typically is mild.4,41 HSV AU is characterised by a more severe anterior segment inflammation.41 The involvement of the vitreous, however, is more prominent in RV, VZV and CMV AUs patients as compared to HSV AU patients.
Iris Changes
Iris heterochromia is considered an important diagnostic feature for RV AU but may also be present in any other VAU.41 Diffuse iris atrophy without heterochromia is also frequently seen in chronic CMV AU.66 As CMV infection is mostly detected in dark-coloured Asian eyes, heterochromia may be overlooked.66 Focal, specifically sectorial, iris atrophy is, however, more characteristic of HSV and VZV AU.12,14,22,60 Posterior synechia is more commonly present in HSV and VZV AU. It is rare in RV and CMV AU.4,41,66
Cataract
Cataract at presentation and iris heterochromia are more common in RV AU and chronic CMV AU.4,41,66
Intraocular Pressure
High intraocular pressure during active inflammation and development of secondary glaucoma is a known complication of VAU. The prevalence of IOP more than 30 mmHg and glaucoma is similar in HSV, VZV, CMV and RV AU.41 However, higher levels of IOP were detected in CMV AU, especially in the acute recurrent (PSS) type.4
Fundus Findings
Focal chorioretinal scars have been occasionally described in RV and VZV AUs.41,82
Laboratory Testing
Since clinical differentiation of the infectious from non-infectious uveitis, and identification of certain causative viral agent may be quite challenging, laboratory testing may be needed. Serological testing for virus antibodies is rarely useful in a patient with VAU. This is because a majority of adults are seropositive for herpesviridea and RV even without a clear clinical history of disease.83 Analysis of aqueous humor is much more valuable than serological testing. Laboratory testing can be performed either by detection of viral DNA/RNA (PCR) or analysis of anti-viral antibodies (Goldmann-Witmer coefficient) in aqueous humor samples. Polymerase chain reaction (PCR) and antibody detection are different testing methods and have different results for different micro-organisms.84 Comparison of PCR versus antibody detection in aqueous humor in anterior viral uveitis is shown in Table 3. PCR in Herpesviridea uveitis and antibody detection in rubella uveitis are probably the most commonly performed laboratory testing methods.6,85 ■