Historically, the first line of treatment of dry-eye symptoms has been various types of eye drops and ointments, including wild cucumber juice containing egg white and goose fat. Water-soluble polymers began to be used in the middle of the 20th century, and gelatin, a denatured collagen, was the earliest natural polymer used in collyria. In the 1960s, synthetic polymers were introduced in artificial tears. In 1974, the US Food and Drug Administration (FDA) decided that the active ingredient of ophthalmic demulcents (lubricants) should be hydrophilic (water-soluble) polymers, and in a monograph determined guidelines to their labeling and composition.
Artificial tears or ophthalmic demulcents remain popular, and the formulation and manufacture of such ‘sterile solutions’ are considered an excellent business opportunity. This is because the market is far from saturated and demand appears to be increasing. The motivation for this, often desperate, search by patients for a more efficacious eye drop is due to the unfortunate fact that conventional products are formulated according to misguided views1 with regard to the major causes of dry-eye conditions. As a result, the efficacy of these eye lubricants leaves much to be desired.
Biophysical Aspects of Tear Film Physiology
Total View of the Tear Film
The unified field theorem2 views the retropalpebral part of the total tear film as a thin, aqueous tear layer covering the frontal segment of the ocular globe. In the open eye, almost half of the area is still hidden in the ocular socket and by the folded upper lid (retropalpebral tear film). This tear layer serves as a lubricant for the rapidly moving upper lids. To avoid tissue damage, hydrodynamic lubrication has to be achieved during blinking. The closing upper lid compresses the superficial lipid layer that remains trapped between the lid edges, which are colored yellow in Figure 1. If the aqueous tear layer is continuous under the lids, colored blue in Figure 1, is at least a few micrometers thick and has low viscosity, the presence of hydrodynamic lubrication will be assured.3
When the eyes are wide open, approximately half of the area of this tear layer is exposed to the atmosphere. When the upper eyelid retracts, the exposed tear layer (about 10μ thick) is immediately coated with a much thinner lipid layer (about 0.1μ in the wide open eye), forming the interpalpebral tear film. The role of this superficial lipid layer is to protect the stability of the underlying tear layer, and it may provide some protection against tear evaporation under extreme circumstances, e.g. air turbulence or low relative humidity.
The role of this dual fluid film is to provide the cornea with an optically smooth refractive surface for the most refractive (corneal) surface of the eye. When the upper lids close, only the superficial lipid layer is compressed between the lids, thus increasing its thickness by 1,000-fold and further lowering the surface tension of the tear film.4
Stability of the Tear Layer
The undisturbed continuity (stability) of the tear layer is of primary importance to safeguard both high-quality (hydrodynamic) lubrication and visual acuity from the lipid-coated segment of the tear layer. The retropalpebral tear layer is contained within two solid surfaces: the globe and the lid. As long as both solid surfaces are hydrophilic,5 the lubricating layer will be stable, remain continuous, and provide the best (hydrodynamic) lubrication. The stability of the interpalpebral tear film requires that the ocular surface covered with the film stays hydrophilic. This condition implies that the cornea–tear interface and the lipid film–air interface have low tension or low free energy per area.
Wetting and De-wetting of Epithelial Surfaces
In simple terms, the ocular surface is completely wetted when it is coated by tears without the assistance of gravity. It also means that the cohesiveness of the tears is less than the adhesiveness of the tears to the epithelium. Such a wet surface can become dry by the evaporation of the water; however, this process requires much energy (heat of evaporation) and it is diffusion-controlled. In fact, the process observed is not one of drying per se but rather de-wetting: instead of spreading over the solid surface, the fluid film ruptures and recedes from it.4
Primary Cause of Dry-eye Symptoms
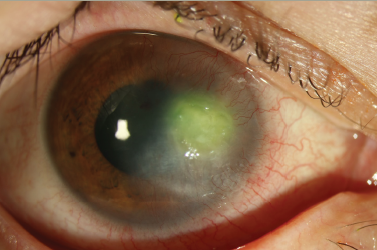
When blinking is prevented, the de-wetting process occurs spontaneously in the eye and results in so-called dry spot formation.6 In fact, the rupture of the tear film may occur at several locations and will increase in size. In almost all dry eyes the tear film prematurely ruptures, i.e. ruptures before the next blink occurs.
When the tear film ruptures, its function is impaired. This can occur both under and between the lids, although it is easier to observe interpalpebrally. It is estimated that almost 90% of dry-eye patients have unstable tear film despite sufficient tear secretion. Discontinuities in the lubricating layer result in boundary lubrication at these places, which would lead to ocular surface damage. Epithelial damage also occurs when the ocular surface is exposed to the atmosphere. Mechanical irritation and exposure could cause sterile inflammation, hence the term for dry eye: keratoconjunctivitis sicca.
Management of Patients with Dry Eyes
The first line of treatment remains the instillation of artificial tears, although some professionals employ punctal plugs to increase the tear volume on a trialand- error basis. This approach may not always be justified since only a minority of dry-eye patients have a diminished tear secretion rate. Unfortunately, the formulation of conventional artificial tears and the selection of the type of artificial tear are often made according to fallacious assumptions.1
Enhanced Viscosity
Elevated viscosity is thought be advantageous in an eye drop. It is assumed to increase residence time and improve lubrication. In fact, increased viscosity increases stress transfer between the moving surfaces and makes lubrication less effective. High viscosity also interferes with the miscibility of existing tears and the spreading of the lipid layer. Furthermore, it does not have a beneficial effect on residence time unless the viscosity is quite high. There are tear substitutes on the market that have a viscosity several hundred times that of tears. They cannot serve as a lubricant and could actually damage the ocular surface. They may work by acting as a semi-fluid lacrimal insert.
Lack of Effect on Ocular Surface Wettability
However, the greatest shortcoming in conventional ophthalmic lubricants has been the inability to wet damaged, and consequently partially hydrophobic, ocular surfaces. As the primary cause of dry eye is the de-wetting of the ocular surface, it stands to reason that an efficacious artificial tear should be able to enhance the wettability of the ocular surface.
Crystalloid Hypo-osmolality
Another fallacy is that a hypo-osmotic eye drop is able to lower the hyperosmotic tear film in dry-eye patients, and that it is advantageous to do so. Since osmolality is a bulk parameter, due to the high tear exchange rate it has only a temporary effect on the tear film properties.7 Furthermore, when the ocular surface tissue becomes damaged and waterlogged, hyper- rather than hypo-osmolality is needed. However, in moderate to severe dry eyes the ocular surface damage may be so great that the surface epithelium loses its semipermeability. In such cases, only colloidal hyperosmolality can remove the excess water.
Formulation of Lacrophilic Artificial Tears
Achieve Complete Wetting
Based on these considerations, an eye drop should be able to achieve the complete wetting of an ocular surface that is at least partially hydrophobic. An eye drop capable of transforming a hydrophobic solid surface so that the eye drop forms a thin stable layer over it (complete wetting) would more than fulfil these criteria.
Dehydrate Leaky Epithelium
Topical solutions containing polymers at high enough concentrations to overcome the imbibition pressure of the corneal stroma are capable of removing excess water even if the cornea is completely denuded. Such formulations with an oncotic pressure greater than 55mmHg are apparently capable of removing excess water from the corneal epithelium and at the epithelium–stroma interface.8
When the polymer concentration in a formulation is increased, the oncotic pressure of the solution will also increase; furthermore, the viscosity of the solution also increases, which interferes with lubrication. Therefore, the polymers have to be carefully selected to reach the desired level of oncotic pressure and still prevent excessive viscosity.
Formulation of the First Lacrophilic Eye Drop (Dwelle®)
An artificial tear was formulated that made a hydrophobic surface completely wettable and also had high oncotic pressure.9 The complete wetting was achieved by developing a polymer mixture that combined two types of polyvinyl acetate: one completely hydrolyzed into polyvinyl alcohol, the other only partially hydrolyzed so that some hydrophobic acetate side chains remained in the molecule. The side chains would adsorb on the plastic or on the dry spots of the ocular surface almost irreversibly by hydrophobic binding.
The hydrophilic groups on the polymer chains, on the other hand, attract the water (of aqueous tears), holding them at the interface. When a solution of these polymers is made at a certain ratio, the solution will completely wet even hydrophobic surfaces. There is a simple test for determining whether an eye drop could wet a hydrophobic surface completely. This test was recently developed by Cindy Brunett, a long-term sufferer from iatrogenic dry eyes.
The Brunett Wetting Test
A plastic cup, e.g. a solo cup, is held sideways so that its upper side is horizontal. Drops to be tested or compared can be lined up along the horizontal line. When the cup is slowly rotated along its longitudinal axis, the drops will roll off on the slope created. If some drops have difficulty in getting started then roll slowly, leaving behind a moist track similar to that of a snail, such a drop is expected to improve the wettability of the ocular surface in dry-eye patients.
Unfortunately, most of the commercially available lubricants fail the Brunett Wetting Test.10 They roll off the cup, leaving it dry. Interestingly, even eye drops that contain intensely hydrophilic polymers will fail the test. On the other hand, Dwelle® (The Dry Eye Company, www.dryeyeshop.com) and related formulations will all form a moist track and thus will pass the Burnett test.
Clinical Testing of Dwelle
The first lacrophilic eye drop was tested extensively in dry-eye patients.11,12 It was named Dwelle because patients soon reported that they did not have to use the eye drop as often as others. A universal finding was the significant decrease of vital staining (by rose bengal or lissamine green). In two-thirds of the patients there was no visible staining after only two weeks of application. The high oncotic pressure of the formulation contributed to the healing of the ocular surface. Patients with recurrent epithelial erosion—a painful, often debilitating condition—also reported that the frequency of erosion has decreased and often disappeared as long as the drops were instilled. This gratifying event occurred even if no bandage contact lens were worn by the patient. Furthermore, Dwelle actually alleviated the condition in cases where bandage lenses had to be worn, so that the patient could eventually be weaned off wearing bandage lenses.8
When carefully administered, two-thirds of a Dwelle eye drop fills the interpalpebral fissure. The only side effect it has is due to its high polymer content, especially when too large an eye drop is instilled: white crystalline deposits could be observed on the eye lashes, which can be readily removed by a moistened tissue. However, patients with severe enough dry eyes ignore such unpleasantness in favor of the relief the drops provide.
Other Lacrophilic Eye Drops13
NutraTear®
Based on the studies on Dwelle, it was a logical step to provide a formulation for marginal and less severe dry-eye patients that contained only the synergistic wetting polymer mixture at low concentration, thus letting the oncotic pressure remain low. A nutrient, cyanocobalamine 0.05%, was added to provide vitamin B12 to the epithelial cells of the cornea. This nutrient is known to enhance epithelial healing and is often used in Europe in traumatized eyes.14 The eye drop, NutraTear® (The Dry Eye Company), provided relief to marginal dry-eye patients and, interestingly, also to patients with red irritated eyes who had been diagnosed as having ‘allergic eyes.’15
Dakrina®
This eye drop is basically Dwelle but also contains vitamin A in the esteric form. The nutrient is made soluble by attaching it to a polymer, similar to the way it is present in the tears. This procedure makes the vitamin A much more bioavailable and more stable. This eye drop has been tested in carefully conducted double-blind clinical trials and found to be effective16 in increasing goblet cell count (density) and reversing pre-keratinization of the corneal epithelium.
Lipid-containing Artificial Tears
With the recognition of meibomian gland dysfunction mostly in iatrogenic dry eyes, artificial tears containing lipid in some form have come into vogue. Tear film instability can also be caused by insufficiency within the superficial lipid layer only.
If one carefully analyzes the mechanics of the superficial lipid layer formation, which is a duplex film, it becomes apparent that the so-called film pressure comprises two components: the surface tension of the lipid layer, which does not usually depend on lipid composition, and the interfacial tension at the lipid–air interface. However, the film pressure can be maximized by decreasing the specific energy at the interface (interfacial tension). This can be achieved by increasing the polar fraction in the lipids. However, this has to be performed carefully because as the interfacial tension approaches zero, the lipid layer will emulsify rather than stay in a duplex film form.
FreshKote® and Clinitas Ultra 3®
These are the trademarks of Dwelle-based formulations (FreshKote®, Focus Laboratories, North Little Rock, Arkansas; Clinitas Ultra 3®, Altacor Ltd, Cambridge, UK) that contain a proprietary lipid blend at a low concentration. The formulation has been tested in clinical trials with positive results by several dry-eye experts in Texas,17 Florida,18 and Australia.19 Currently, these are marketed in the US and the UK and will soon be available in other countries in Europe.
Conclusions
Clinical studies and patient experience with Dwelle suggest that the biophysical properties of superior wetting and high colloidal osmolality, rather than the eye drops having high viscosity or low crystalloid osmolality, are important in determining the clinical efficacy of aqueous collyria in the amelioration of dry-eye conditions and repair of corneal epithelium. Dwelle has also been proved useful as a vehicle for solubilized retinyl palmitate for use in mucin-deficient dry eyes and also for a phospholipid for dry eyes with meibomian gland dysfunction.