The structural properties of collagen framework in the corneal stroma determine the biomechanical and optical properties of tissue. Optimal corneal optics requires a smooth, regular surface with a healthy tear film and epithelium. The regular arrangement of stromal cells and macromolecules is necessary for clear vision. The lattice arrangement of collagen fibrils embedded in the extracellular matrix acts as a diffraction grating to reduce light scattering by means of destructive interference. Scattering is greater anteriorly, resulting in a higher refractive index that decreases from 1.401 at the epithelium to 1.380 in the stroma and 1.373 posteriorly. With normal collagen regulation we can see clearly because the lattice elements are smaller than the wavelength of visible light.1 This is disrupted in keratoconic corneas owing to loss of arrangement of fibrils in the anterior stroma, a decrease in the number of collagen lamellae and separation of collagen bundles.2,3 A new treatment based on collagen cross-linking (CCL) has now been introduced by Wollensak.4,5 This new treatment is aimed at the pathogenic cause of keratoconus and changes the intrinsic biomechanical properties of corneal collagen.
This treatment creates additional chemical bonds inside the corneal stroma by means of photopolymerisation in the anterior stroma while minimising exposure to the surrounding structures of the eye.6 Crosslinking is widely used in the polymer industry to harden materials and in bioengineering to stabilise tissue. For example, chemical crosslinking with glutaraldehyde is used in the preparation of prosthetic heart valves, and physical cross-linking by ultraviolet A (UVA) is often used in dentistry to harden filling materials.5,7 In pathology, the same method is used to preserve and harden tissue specimens by glutaraldehyde or formaldehyde.
The photosensitiser is excited into its triplet state, generating so-called reactive oxygen species (ROS) – mainly singlet oxygen and, to a much lesser degree, superoxide anion radicals using UVA at 365nm and the photosensitiser riboflavin. The ROS can react further with various molecules, inducing chemical covalent bonds bridging amino groups of collagen fibrils (type II photochemical reaction). The wavelength of 365nm was chosen because of the absorption peak of riboflavin at this wavelength.8
A significant challenge in drug delivery is the local administration of drugs to the eye.9,10 To be effective, most drugs must penetrate across the eye’s tissue barriers (cornea, sclera and conjuctiva) to reach therapeutic targets within the globe. Often, these tissues present the rate-limiting step to effective delivery. Thus, the ability to predict rates of drug transport across ocular tissues would be a powerful tool in the development of new drugs and drug delivery strategies.10
Surgical Technique
Removal of Epithelium and Cornea Permeability
A number of centres around the world are now performing corneal CCL treatment with removal of the epithelium, as first described by the authors. The cornea contains three primary layers that are stacked sequentially from the outer to the inner surface: epithelium, stroma and endothelium. In the human eye, the epithelium contains five to seven layers of cells, each connected by tight junctions, which are expected to provide a large barrier to anything but small lipophilic compounds. In normal eyes, the stroma is a thick, fibrous, largely acellular tissue composed mostly of water, which should not provide a lipophilic barrier. Finally, the endothelium is a monolayer of cells with large intercellular junctions, which should present a leaky lipophilic barrier. The resistance to transport across the whole cornea can be thought of as a sum of resistances to transport across each of the individual corneal layers, where the resistance to transport (R) is the inverse of permeability (P):
R cornea = R epithelium + R stroma + R endothelium.
Using this ‘sum of resistances’ approaches allows us to determine which layers of the cornea provide rate-limiting barriers by comparing the permeability of the full cornea with the permeability of the cornea with one or more of its layers removed. For example, if the permeability of the full cornea was found to be smaller than that of the de-epithelialised cornea, this would suggest that the epithelium presents a significant barrier to transport. In contrast, if the permeability of the full cornea was found to be equal to that of the de-epithelialised cornea, the epithelium does not present a significant barrier to transport.
When the stromal layer of the cornea is isolated, its permeability shows no apparent dependence on molecular radius, as expected for its anatomical structure. Because whole cornea and corneal stroma have such different permeability properties, it at first appears that the stroma is not a rate-limiting barrier within the cornea.
The permeability of the endothelial layer of the cornea displays a strong dependence on both distribution co-efficient and molecular size. This indicates that both the lipophilic pathway across cells and the hydophilic pathway between cells are important. To determine whether the endothelium is a rate-limiting step for transport across the full cornea, the permeability of the endothelium can be compared with that of the cornea. For molecules with the same distribution co-efficient, endothelial permeability is generally larger than that of the cornea, indicating that the endothelium is more permeable and, thus, not a rate-limiting barrier.
Neither the stroma nor the endothelium is uniquely rate-limiting, but each can play a role in limiting transport of small lipophilic compounds. By process of elimination, this leaves the epithelium as the dominant barrier in the cornea. Almost no permeability data exist in the literature for the corneal epithelium alone. If we accept that the epithelium dominates the cornea’s barrier properties, it still remains unclear which of the other layers (stroma, endothelium) is the second most important barrier.10
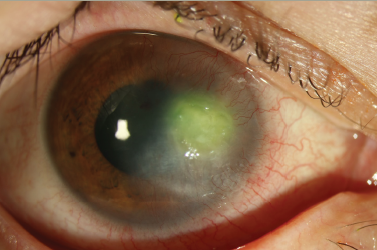
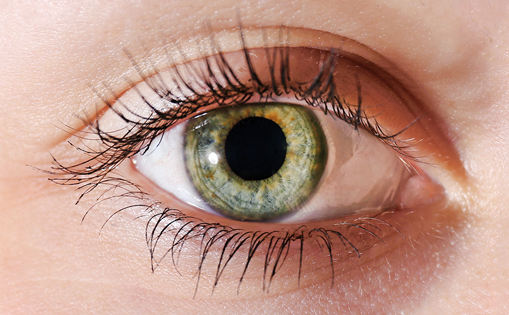
Non-removal of the epithelium has considerable benefits in terms of post-operative pain and more rapid healing. Some complications have been reported in the literature after CCL treatment with removal of the epithelium, such as herpetic keratitis with iritis.11Figures 1 and 2 show confocal biomicroscopic views of normal epithelium and change after 20% alcohol application, respectively. In Figure 2 there is no intact epithelial membrane, and no tight junctions are expected. The intact epithelium is a barrier that slows the absorption of riboflavin (molecular weight 376.37g/mol) into the cornea so that it penetrates slowly and incompletely. For this reason, chemically disturbed epithelium (by application of 20% alcohol) or debrided epithelium removes the diffusion barrier for the riboflavin molecule and speeds up saturation of the corneal stromal tissue.10,12
An important point to remember is that while riboflavin reduces UV penetration by absorbing it, the absorption then results in a reaction that causes the cytotoxic reaction. In fact, the presence of riboflavin makes the cornea 10 times more UV-sensitive. It would be ideal if the riboflavin penetration could be limited to the first 300μ of the cornea, as this would limit the photochemical reaction to this level and thus ensure protection of the endothelium.13
Under sterile conditions, 20% alcohol is applied for 25 seconds, similar to the laser epithelial keratomileusis (LASEK) procedure. Initially, 0.5% proparacaine and 2% pilocarpine eye drops are administered every two minutes and every five minutes, respectively, for 30 minutes; miosis is used as anaesthasia in order to minimise exposure of the lens and decrease photosensitivity. Next, riboflavin drops (0.1% riboflavin-5- phosphate and 20% dextran) are administered every three minutes for 30 minutes. Penetration of riboflavin to the corneal stroma and anterior chamber is confirmed by slit-lamp examination. The CCL procedure is then performed by exposing the central 7.0mm of the cornea to UVA light (3.0mW/cm2 at 365m), for 30 minutes. This is combined with continued topical application of riboflavin solution (0.1% riboflavin-5- phosphate and dextran) every three minutes, without removing the epithelium (see Figure 3), similar to the technique described by Chan et al.14 Keeping the epithelium intact led to less patient discomfort after the procedure. After treatment, artificial tears are used for a few days.
Clinical Results
An early clinical study on the cross-linking treatment of keratoconus was performed by Wollensak.4 This new treatment is aimed at the pathogenic cause of keratoconus and changes intrinsic properties of corneal collagen. In this three-year study, 22 patients with progressive keratoconus were treated with riboflavin and UVA. CCL had a favourable effect on all treated eyes. In 16 eyes (72%) there was also a slight reversal and flattening of the keratoconus by 2 diopters (D). Best corrected visual acuity (BCVA) improved slightly in 15 eyes (68%). According to the results of cross-linking treatment, regression of the disease was achieved in 70% of eyes, with a reduction of the maximal keratometry readings by 2.01D and of the refractive error by 1.14D.4 Caporossi et al.15 showed a mean K reduction of 2.1D, and Braun et al.16 reported stabilisation of keratoconus in all 22 patients and 27 eyes and regression by 2D in 12 eyes (44%) after CCL treatment.
Chan et al.14 reported the first study about combined treatment with Intacs and CCL. They showed that the combination of CCL with Intacs led to better results than Intacs insertion alone, as proved by greater reductions in manifest refraction, steep K and average K. In their study, mean changes in uncorrected visual acuity (UCVA), BCVA, sphere and mean K values were 6.5 lines, 1 lines, 0.12D and 1.34D, respectively, after Intacs with CCL, and 9.5 lines, 1 line, 0.25D and 0.21D, respectively, after Intacs treatment only. They concluded that this might be the result of biomechanical coupling from local collagen changes around the segments. The response to cross-linking alone was not evaluated in comparison with the combined method.
Cross-linking with the epithelium removed versus transepithelial treatment is another controversial issue. Cross-linking treatment without removing the epithelium leads to inadequate penetration of riboflavin and therefore enhances UV penetration, possibly resulting in cell damage. Pinelli et al.17 reported their six-month cross-linking results and found comparable outcomes without removal of the epithelium in terms of changes in keratometry, vision and endothelial cell count. Sharma and Boxer Wachler18 also reported similar results after cross-linking without removing the epithelium. Podskochy et al.19 showed increased keratocyte damage with UV light when the epithelium was removed. This study reported that epithelium may play a significant role in absorbing UVA, thus protecting the cornea and deeper structures from damage.
Table 1 summarises clinical results from different centres, including the reports with an increase in K values in some cases after CCL treatment. We have seen dramatic improvements in visual acuity values without change in corneal topography in some of our cases (see Figure 4). These observations show us that improvement in visual acuity may perhaps be unrelated to the change in corneal shape and mean K values. It may in fact be due to a change in stromal refractive index or optical regularisation of the central cornea as a result of collagen cross-linking,13 as listed in Table 2.
Complications
Riboflavin is a key component of photochemical cross-linking treatment as it increases corneal absorption of UVA to approximately 95%, thereby protecting the deeper ocular structures – especially the endothelium – from UVA damage.20,21 The damage from UVA depends on its wavelength, its irradiance and the irradiation time.22 Photokeratitis has been shown to occur in the cornea at wavelengths of 270–315nm (UVB), with dose densities ranging from 0.12 to 0.56J/cm2. Cataract development has been presented for wavelengths between 290 and 365nm in the literature.23,24 Thermal- or blue-lightinduced photochemical damage in the wavelength range of 400–1,400nm damages the retina.25
In the cross-linking treatment, a 365nm UVA spectrum is used. To avoid danger to the endothelium, lens or retina, it is necessary to perform pre-operative pachymetry in every patient to exclude extended areas with a stromal thickness of less than 400μ and to check the UVA irradiance precisely using a UVA-meter.6 Stromal haze, which is common when the epithelium is removed, and herpetic keratitis with iritis have been reported in the literature as complications after CCL treatment in keratoconic eyes.11,26
Keratocyte damage is not considered a major issue as many other corneal procedures, including excimer laser refractive surgery, involve keratocyte damage at similar depths, with repopulation by migrating keratocytes occurring by six months with no long-term consequences noted.27,28 Caparosi et al.29 studied 10 eyes with confocal microscopy after UVA riboflavin and found well-demarcated vertical and lateral transition zones at 270–300μ. The anterior stroma showed oedema with only a few keratocyte nuclei and poor reflectivity, whereas the posterior stroma showed regular keratocyte population and normal reflectivity. Repopulation of keratocytes started at one month after treatment and was completed by six months after treatment, with the corneal endothelium showing normal morphology up to six months after treatment.
Conclusion
We do not yet know the real effect of CCL treatment, but we can tell that CCL treatment may change corneal intensity, corneal function and corneal rigidity, but not corneal shape. This procedure can be used to prevent keratoconus progression for stability.