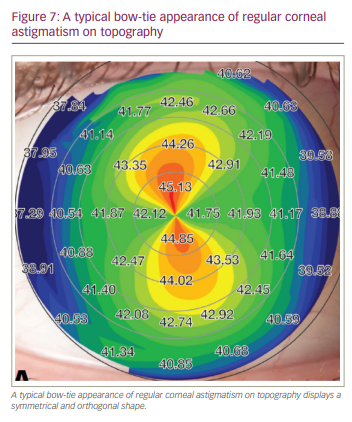
Excess corneal astigmatism can cause visual aberrations, resulting in symptoms of glare, starbursts and halos. Astigmatism has long been difficult to correct with refractive laser surgery. The challenge has been to maximally reduce both corneal and refractive astigmatism while ensuring that any remaining corneal astigmatism is regular, symmetrical and orthogonal, with a typical ‘bow-tie’ topography.1 However, such perfecting treatment for both regular and irregular astigmatism is now possible. By conceptually dividing the cornea in two, treatment can be customized for each half. Therefore, corneal astigmatism can be optimally reduced and regularized in a single step – leaving the cornea symmetrical and orthogonal – while also targeting plano-refraction. Such
hemidivisional treatment has the potential to improve best-corrected visual acuity, as well as reduce higher order aberrations, and can be done using laser-assisted in situ keratomileusis, photorefractive keratectomy or small in situ lenticule extraction procedures.2
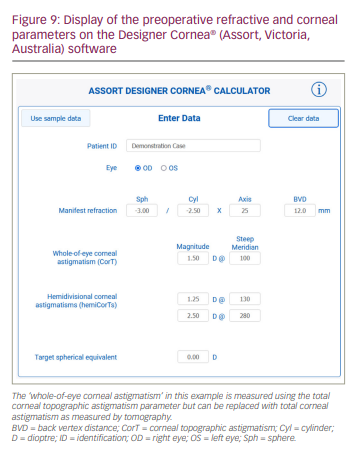
Treatment parameters are calculated with the Designer Cornea® (Assort, Victoria, Australia) software, which is freely available online at www.assort.com or www.isrs.org for members of the International Society of Refractive Surgery. This calculator is for investigational use only and should be used in conjunction with excimer or femtosecond refractive laser device manufacturers.The Designer Cornea software applies the vector planning method to each half of the cornea, correcting for any associated myopia or hyperopia and targeting a spherical equivalent of zero for spectacle refraction. By incorporating corneal parameters into the refractive treatment plan, the ocular residual astigmatism (ORA) can be calculated to minimize corneal and refractive astigmatism.3–6
ORA is the amount of astigmatism that remains in the refractive system of the eye and its correction after surgery, regardless of how well the procedure is performed.3,4 It is defined as the vectorial difference between the refractive cylinder at the corneal plane and corneal astigmatism measured in dioptres (D).3,4 Significant ORA (i.e. >1.00 D) has been shown to be prevalent in as much as 45% of the German population.7 ORA is caused by preoperative corneo-refractive differences in the magnitude and orientation of any astigmatism and must be calculated for all patients before undergoing refractive laser eye surgery. This will enable the surgeon to determine how much of the astigmatism can be treated and to manage the patient’s expectations effectively.
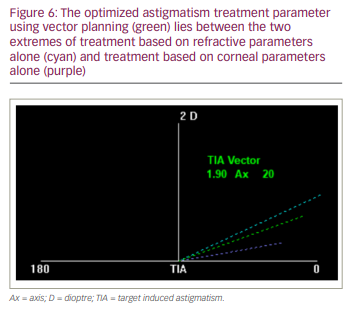
Vector planning addresses the corneo-refractive difference by considering both corneal astigmatism and the refractive cylinder in the treatment plan, emphasizing ORA to minimize both parameters. Vector planning also has an inbuilt safety mechanism, which ensures that, the greater the disparity between the corneal and refractive astigmatism in magnitude and/or orientation, the less the astigmatism treatment (target-induced astigmatism [TIA] vector) is applied. This avoids the possibility that the ORA exceeds the preoperative measurement, which would leave the patient with more corneal astigmatism than they had before the surgery.
The application of vector planning to the whole eye can be shown by way of an example.
If preoperative, manifest refraction is -3.00 DS/-2.50 DC x 25 (12 mm), and total corneal topographic astigmatism (CorT Total) is 42.00 D/43.50 D @ 100, then the calculated ORA is 1.22 D axis (Ax) 134 (Figure 1 and Figure 2).
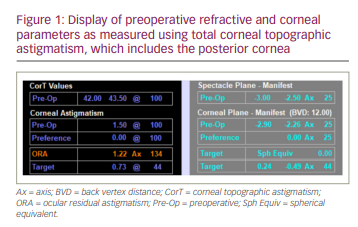
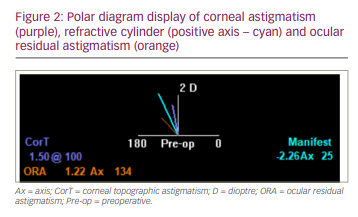
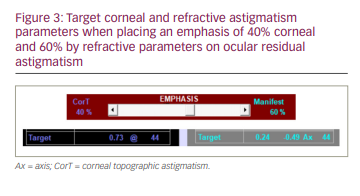
Placing a 60% emphasis by refractive parameters on ORA results in a corneal target of 0.73 D @ 44 and a refractive cylinder target of -0.49 D x 44. Note that these two magnitudes of topographic plus refractive astigmatism add to the ORA magnitude of 1.22 D and that the targeted spherical equivalent is zero (Figure 1 and Figure 3).
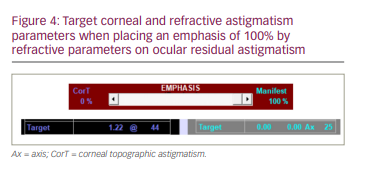
Treatment using 100% emphasis on the ORA, as is customary in most practices,8 will target a refractive cylinder of zero but leave all the ORA, 1.22 D, on the cornea (Figure 4).
Treatment parameters based on topography-guided measures will place the emphasis at 100% by corneal parameters. This will target all the 1.22 D ORA in the postoperative refraction, potentially leaving the patient requiring refractive correction (Figure 5).
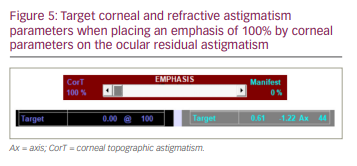
Figure 6 displays astigmatism treatment (TIA vector) parameters based on either refractive cylinder alone (cyan) or corneal parameters alone (purple). Alternatively, the green line shows the treatment based on vector planning; in this case, an emphasis of 60% by refractive parameters on the ORA lies between the two extremes.
Current refractive laser treatments using vector planning are based on one chosen refraction (manifest or wavefront) and one measure of corneal astigmatism.4,5 This approach works well but can be further customized to improve outcomes not only when correcting regular astigmatism, where the typical topography is that of a symmetrical, orthogonal bow-tie pattern (Figure 7), but also for irregular astigmatism, where the bow-tie shape is non-orthogonal, asymmetrical or both (Figure 8).
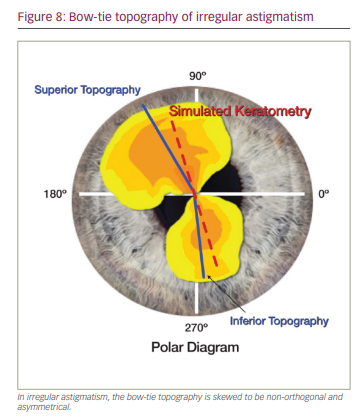
As mentioned previously, when planning refractive astigmatism laser treatment, the bow-tie appearance can be divided in two to produce two measures of corneal astigmatism. Vector planning can now be applied to both halves of the cornea using the common refraction to both.9,10
The cornea is conceptually halved using the flat orientation of the total corneal astigmatism. Any measure of total corneal astigmatism can be used; however, the example here is based on CorT Total. CorT Total has been shown to be more accurate than CorT Anterior, simulated keratometry and other measures of corneal astigmatism that include the posterior cornea.11,12
By using tomography, a measure of astigmatism can be obtained for each half of the cornea. For example, on the CSO Sirius topographic system (Costruzione Strumenti Oftalmici, Firenze, Italy), these measures can be obtained from the ‘hemi-meridians’ section, which displays a pair of steep and a pair of flat magnitudes with orientation using the 5 mm zone, while using one common refraction for each half of the cornea.
By using vector planning separately for each half of the cornea, the astigmatism treatment can be further customized to optimally reduce corneal astigmatism and refractive cylinder and to regularize any remaining corneal astigmatism by targeting a symmetrical and orthogonal cornea (Figure 7).
Let’s again consider the previous example: the manifest refraction is -3.00 DS/-2.50 DC x 25 (12 mm), and CorT Total is 1.50 D @ 100. Conceptually, the cornea is halved along the flat corneal meridian of 10 degrees, and vector planning is applied separately to each half (Figure 9). The first step requires the maximum reduction of astigmatism, which accounts for corneal and refractive parameters. Using the corneal measures (from tomography) of 1.25 D @ 130 for one half of the cornea together with the +2.26 D x 115 (note conversion to positive cylinder) refractive cylinder at the corneal plane, ORA is calculated as 1.34 D Ax 101. Similarly, for the other half of the cornea, where the astigmatism is measured as 2.50 D @ 280, and common refractive cylinder is also +2.26DC x 115, the ORA is calculated as 1.25 D Ax 158.
The emphasis on ORA can vary from 100% emphasis on totally correcting refractive cylinder to 100% emphasis on totally correcting CorT (topography-guided treatment). Previous studies have shown that an average 60% emphasis by refraction and 40% emphasis by corneal parameters work well for most cases.4–6 However, the surgeon can vary the emphasis on ORA separately for each half of the cornea to optimally reduce corneal astigmatism, leaving any remaining astigmatism depending on how favourable its targeted orientation may be.
Figure 10 shows a polar diagram displaying the corneal and refractive parameters for each corneal half, as they would appear on the eye before and after surgery. The astigmatism treatments required to optimally reduce astigmatism can be displayed by checking the ‘show reduction TIA’ box.

The next step involves regularizing the cornea. This is achieved by targeting the vectorial average of the corneal targets (from the reduction step above) for each half, which will result in a symmetrical and orthogonal cornea. Figure 10 also displays the expected postoperative corneal and refractive targets after regularizing the astigmatism, as well as all possible corneal targets (yellow) for the different emphasis options available for each half. For simplicity, an emphasis of 60% by refractive parameters on ORA has been chosen in this example for both halves. The treatments needed to regularize the cornea can be displayed by checking the ‘show regularisation TIA’ box.
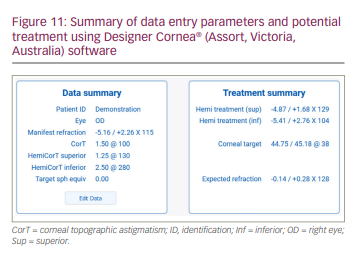
Figure 11 displays the numerical values of the treatment parameters for each corneal half together with the orthogonal corneal target at a meridian of 38 degrees and an expected refractive target of -0.14 DS/+0.28 DC x 128. Note the refractive target of a spherical equivalent of zero.
Hemidivisional vector planning to reduce and regularize astigmatism by laser treatment can be used on all types of astigmatism: regular and irregular with spherical refractive error. This advanced treatment can be performed in one step, simultaneously combining the reduction and regularization processes and leaving any remaining minimized corneal astigmatism in a regular state. The excimer and femtosecond manufacturers can now look at further customizing their lasers to offer this treatment to all their doctors.







