Since the first description of glaucomatous optic neuropathy (GON) by von Graefe, there has been debate about the pathomechanisms involved in this damage. In the discussions that followed two questions were of great interest: first, how far is the damage a consequence of mechanical stress on the optic nerve head (ONH), and second, to what extent is it due to circulatory insufficiency? This short article aims to answer these questions.
Phenomenology of Glaucomatous Optic Neuropathy
For the clinician, the most striking difference between GON and other types of optic neuropathy is ONH excavation. However, there are a number of additional, partially unspecific, morphological features of GON, including the loss of retinal ganglion cells, thinning of the retina and optic nerve, shrinking of the lateral geniculate nucleus, cell loss in the visual cortex, ‘splinter haemorrhages’, peripapillary atrophy and activation of glial cells both in the ONH and in the retina. However, there are also a number of systemic changes, leading to the designation of glaucoma as ‘a sick eye in a sick body’.
Risk Factors for Glaucomatous Optic Neuropathy
An indisputable risk factor is intraocular pressure (IOP); however, there is mounting evidence in literature that other risk factors are involved as well. These additional factors may by themselves lead to GON, or may render the eye more sensitive to IOP. Among the most often described factors are thin cornea, low blood pressure and vascular dysregulation. Low blood pressure and vascular dysregulation are not independent factors, because on the one hand patients with a vascular dysregulation syndrome often suffer from low blood pressure, and on the other hand patients with vascular dysregulation often have disturbed autoregulation, which renders the eye more sensitive to both an increase in IOP and a decrease in blood pressure.
Circulation and Glaucomatous Optic Neuropathy
Using different methods, many research centres have reported reduced blood flow or at least reduced blood-flow velocity in different parts of the eyes, but also behind the eyes in the retro-ocular vessels and even in the brain and in the fingers, particularly in glaucoma patients who progress despite a normal or normalised IOP.1 Some of the reduction in blood flow may be secondary to either an IOP increase or the glaucomatous damage. However, the fact that reduced blood flow can be observed even in the nailfold capillaries indicates that there must be an additional primary component involved. At first glance, these findings seem confusing as reduced ocular blood flow (OBF) occurring in the context of other diseases, e.g. multiple sclerosis (due to a high level of circulating endothelin [ET]), does not apply to GON, although it often leads to some atrophy of the ONH. Furthermore, classic risk factors for disturbed circulation such as smoking, dislypidaemia, diabetes, etc., although statistically weakly related with an increased IOP, do not seem to be independent risk factors for GON. Before we attempt to understand these observations, we will describe some of the basic aspects of blood flow and particularly of OBF.
Regulation of Blood Flow
Blood circulation serves to transport a large variety of molecules including oxygen, cells such as leucocytes and heat. Regulation of blood flow is necessary to adapt to the varying internal and external conditions. During exercise, for example, the oxygen demand of the muscles increases dramatically. When we move quickly from a warm to a cold environment, our circulation adapts to redistribute body temperature in order to avoid too much heat loss through the skin and, as an example, to keep the temperature of the back of the eye constant.
The overall blood flow in the body is regulated by the cardiac output, which is mainly controlled by the autonomic nervous system and circulating hormones. However, the distribution of this cardiac output to different organs or parts of organs is regulated by the relative local resistance to flow.
Regulation of Local Resistance in the Eye
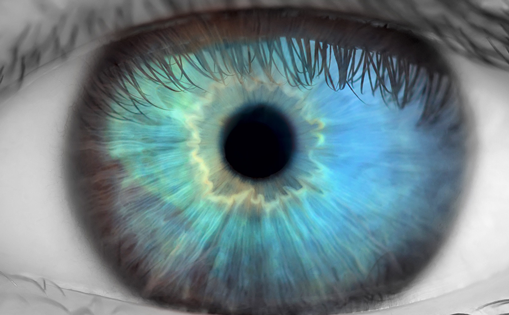
The vessels of the eye are, similar to all other blood vessels, controlled by the vascular endothelial cells (VECs), which release vasoactive molecules. The most important molecule is nitric oxide (NO), which induces vasodilation; another is ET-1, which leads to vasoconstriction. In addition, the vessels of the retina and the ONH are influenced by the activity of the neural and glial cells (so-called neurovascular coupling). The chorioidal vessels are mainly controlled by the autonomic nerve system. Due to the blood–retinal barrier, circulating hormones such as ET-1 or angiontensin II have no direct access to smooth-muscle cells (SMCs) and pericytes; therefore, they have relatively little effect on retinal circulation (see Figure 1). The situation is different in the choroid, which has fenestrated capillaries. Even larger molecules, such as hormones, escape the vessels and obtain direct access to SMC. These hormones in the choroid can also diffuse, to some extent, into the ONH.2
Circulating Hormones and Splinter Haemorrhages
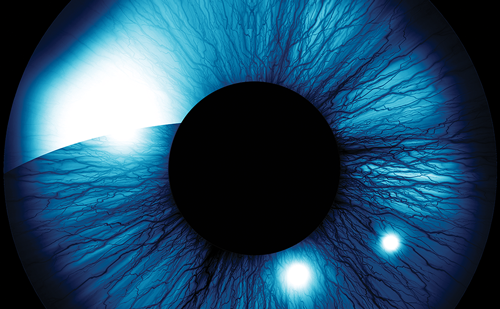
Circulating molecules such as ET, vascular endothelial growth factor (VEGF) or matrix metalloproteinases (MMPs) can diffuse from the choroid into the ONH and neighbouring retina and reach the vessels from the outside. In this way, they are also able to influence the blood–brain barrier, which in extreme situations is weakened to such an extent that even erythrocytes are able to escape from the vessels. This leads to the so-called splinter haemorrhages at the border of the ONH (see Figure 2).3
The Oxygen Paradox
Oxygen is crucial for the survival of tissues, but at the same time it is also potentially very toxic. Reactive oxidative species (ROS) damage the cell structures. ROS are mainly produced in the mitochondria. ROS production depends on the local oxygen tension and on electrical potential of the mitochondria.4 The latter is a proportional function reduced to oxidised redox carrier in the respiratory chain. If oxygen supply is more or less constantly reduced (e.g. in cases of arteriosclerosis or of multiple sclerosis), the tissue can adapt to some extent. However, if the oxygen supply is low, tissue infarction may result. A slight and short drop in oxygen supply leads to what is termed ‘preconditioning’. In this way, the tissue can better tolerate subsequent decreases in oxygen. If the oxygen decrease is stronger, ROS production can exceed the organism’s capacity to cope with free radicals. As a consequence, oxidative stress damages cellular structures. To some extent, these cellular structures can still be repaired; however, if the induced damage exceeds the capacity for repair, structural damage will remain. After repeated insults, the structural damages build up, ultimately leading to clinically detectable disease.
Vascular Dysregulation
An insufficient oxygen supply to a certain tissue can be due to a structural damage of the vessels (e.g. an atherosclerosis or thrombosis) or due to vascular dysregulation. Such a dysregulation can be local (e.g. due to a local dysfunction of the endothelial cells) or may be more or less systemic. The term vascular dysregulation syndrome in the context of glaucoma was first introduced by Flammer.5 Later, a distinction was made between primary and secondary vascular dysregulation. A systemic vascular dysregulation can be secondary to another disease, e.g. secondary vascular dysregulation (SVD) in multiple sclerosis.6 However, primary vascular dysregulation (PVD) occurs in otherwise healthy subjects. While subjects with SVD have a reduced baseline OBF, subjects with PVDhave compromised autoregulation of ocular perfusion. This explains why SVD is a weak and PVD a strong risk factor for glaucomatous damage. A PVD can often be observed particularly in patients with normal-tension glaucoma (NTG). For this reason, PVD will be discussed here in some detail.
Primary Vascular Dysregulation
PVD syndrome is characterised by an inborn tendency to respond differently to a variety of stimuli such as feeling cold or emotional or physical stress. The symptoms may already be present in childhood, but become clearly manifest during puberty and mitigate as subjects get older, in particular during menopause. The syndrome is observed more often in females than in males, in slim rather than in obese people, in professionals rather than in blue-collar workers and in Asians rather than in Caucasians. The leading symptom in PVD is cold extremities.
In addition, their feeling of thirst is also reduced. These subjects normally drink enough only because they know that they have to drink, rather than because they feel thirsty. They also have a prolonged sleep-onset time, which is due to the fact that there is a strong connection between feet temperature and sleep-onset time. PVD subjects also have an altered drug sensitivity. This is at least partially due to altered gene expression of the ABC transport proteins. PVD subjects often have low blood pressure when they are young, particularly at night. Moreover, the ET level in their circulating blood is increased, and the sensitivity to ET is bloodpressure- dependent. PVD patients more often show splinter haemorrhages, reversible diffuse visual field defects and clinical signs of activated astrocytes in the retina. In terms of circulation, their retinal vessels show a higher spatial irregularity and are stiffer, and vasodilation to flickering light is reduced. The autoregulation (adaption to changes in perfusion pressure) of OBF is disturbed. This is the major link to glaucoma. PVD subjects have a higher risk of various eye diseases but particularly for glaucoma.7
Primary Vascular Dysregulation and Autoregulation
There is increasing evidence that GON is related more to an unstable OBF than to a constant blood-flow reduction. OBF is unstable if either IOP fluctuates on a high level (sometimes exceeding the autoregulation capacity) or autoregulation itself is disturbed. For decades, defective autoregulation of OBF in glaucoma patients has been postulated, but only recently could this be demonstrated. The main cause of disturbed autoregulation is a PVD syndrome. The involvement of PVD explains why systemic hypotension in these subjects (but less so in others) is a risk factor for GON, why females suffer from NTG more often than males (females suffer more often from PVD) and why NTG occurs more often in the Japanese than in Caucasians (Japanese suffer more often from PVD), but also why NTG patients and females have splinter haemorrhages more often.
Pathogenetic Concept
The above-described facts led to the following pathogenetic concept: both mechanical and ischaemic stress activate the glial cells, leading to an altered microenvironment, particularly in and around the ONH (see Figure 3). This includes increased production of MMPs, which are involved in tissue remodelling. In addition, the activation of astrocytes leads to increased NO production. Although it has a short half-life, NO is small and liposoluble and can, therefore, readily diffuse to neighbouring cells such as the axons of the ONH.
In parallel, recurrent mild reperfusion leads to the production of the superoxide anion (O2 .-) in the mitochondria, which is copiously located in the axons of the ONH. In this situation, the superoxide anion (O2 .-) can readily combine with NO to produce the highly damaging peroxynitrite (ONOO-), which in turn, induces apoptosis.8 Blood flow and, consequently, oxygen supply is unstable if IOP fluctuates at a relatively high level or if autoregulation is disturbed. In turn, autoregulation is disturbed in cases of PVD syndrome. PVD can also lead to low blood pressure and thereby further contributes to GON.
Conclusions
The pathogenetic mechanisms that lead to GON are only partially known. Obviously, a number of factors and mechanisms are involved. These factors are most likely inter-related, as in a ‘complex network’. Therefore, it not a question of whether glaucomatous damage is more likely due to one or the other factor (e.g. pressure versus vascular factors), but rather a question of how these and other factors interact in a patient. The elucidation of these factors in the future will hopefully lead to the development of new treatment strategies.