The moment the first person steps on Mars will be one of the most unifying and defining moments in human history. Mars is the closest planet to Earth and is 35 million miles away at its closest point and 250 million miles away at its furthest point. A one-way trip to Mars would take 7 months and expose astronauts to incredible stresses on the body. As we all know, the effects of ionizing radiation, bone demineralization, muscle loss, and the psychological impacts of long-term space flight are hard to overstate. Numerous counter measures have been developed so that humans can survive the harshest environment imaginable in an entirely manmade confinement system. A recently described condition, known as VIIP (visual impairment and intracranial pressure [ICP]) poses an immediate risk to astronauts’ vision during long term space flight.
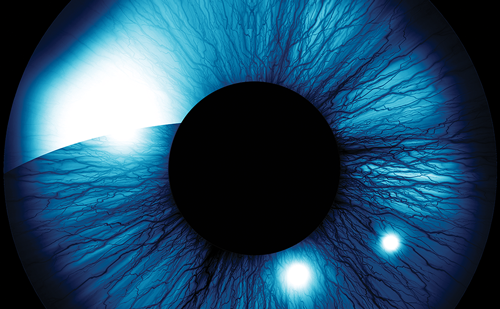
As ophthalmologists, we often think of the eye in isolation. We perform cataract surgery, or glaucoma surgery, or retinal surgery and are sub-specialized to millimeters of the body and sometimes subspecialized to microns. Often times we can lose perspective that the eye is an extension of the body and rarely do we think past 30 mm and how the eye interacts with the brain and the body as a whole. Because we are so focused, we have become tremendous at what we do. Surgeons can do cataract surgeries, and cornea transplants, and orbital surgeries, and retinal surgeries with incredible efficiency, safety, precision, and tremendous outcomes, but through our sub-specialization, we have forgotten many of the things that we were taught in medical school and early anatomy classes. In fact, many ophthalmologists, if asked, would not know that the cerebral spinal fluid bathes the optic nerve all the way to its insertion into the posterior globe. We often think of only the visible portion of the optic nerve, but of course it is actually long connection between the eye and the brain. Perhaps our neuro-ophthalmology colleagues think of the retrolaminar optic nerve frequently, but a glaucoma specialist rarely does, even though their existence is dedicated to the optic nerve. Because of we have focused on the visible and readily studiable portion of the optic nerve, we have not spent adequate resources understanding the interaction between intraocular pressure (IOP) and ICP. Recent studies have shown that the relationship between IOP and ICP may be fundamental in the pathogenesis of glaucoma, and caused by either a high IOP or low ICP.1,2 For example, if the IOP is normal, but the ICP is low, a pressure differential across the optic nerve head exists and normal tension glaucoma can ensue. Conversely, in ocular hypertension, a patient may have a high IOP, but also a high ICP, and be protected from developing glaucoma despite having high IOP. In idiopathic intracranial hypertension, the ICP becomes higher than the IOP and the optic nerve bows forward and there is axonal transport that is slowed at the level of the lamina cribrosa and you see swelling of the optic nerve head anteriorly. As we understand more about the role that pressure balances play across the optic nerve, new insights into the basic pathophysiology, in addition to new therapeutic targets emerge. This has significant implications for VIIP.
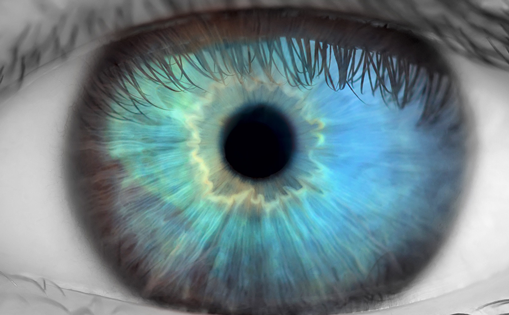
VIIP is a syndrome that consists of posterior globe flattening, a hyperopic shift, papilledema, and choroidal folds. This syndrome was not identified until astronauts spent extended periods on the International Space Station. The physiology behind VIIP is likely multifactorial because of the significant fluid shifts and cardiovascular changes in the body during long-term space flight, but it is currently primarily attributed to an elevated ICP. VIIP was not describe on short-term space flights, such as the shuttle missions, because the duration was likely not enough to start to develop the symptoms of VIIP. However, longer duration space flights, such as the 6–12 month time periods that are spent on the International Space Station, allowed enough time for this syndrome to be observed. Approximately 50% of astronauts on the International Space Station demonstrate one or more signs of VIIP. The basic physiology is that on Earth in a gravity-filled environment, our cerebral spinal fluid and other bodily fluids, are pulled down caudally by gravity. In space and in the absence of gravity, the fluids of the body, including cerebral spinal fluid, redistribute cranially. This leads to a cerebrospinal fluid (CSF) pressure at eye level that is higher than normal. This elevated ICP at eye level results in filling of the optic nerve subarachnoid space with cerebral spinal fluid and anteriorly directed forces on the optic nerve and the posterior globe. This increased CSF pressure results in flattening of the posterior globe, which in return results in a hyperopic shift because of the shortened axial length. One can imagine with all of the intricate instrumentation at arms’ length, a hyperopic shift can pose significant obstacles on long-term space flight and that is one reason why adjustable glasses have been developed for astronauts to use while in space. Additionally, papilledema ensues, most likely because the ICP is now elevated beyond typical IOP and orthograde axonal transport cannot travel from the ganglion cell bodies in the retina toward the brain and the lateral geniculate ganglion. The axonal transport materials are blocked at the level of the lamina cribrosa and accumulate and cause swelling of the optic nerve. Finally, because of the globe flattening, the choroidal folds are seen because the volume of the eye is a bit smaller and retinal and choroid do not change shape so it is analogist to a carpet in a room that was made smaller and it bunches up.
The National Aeronautics and Space Administration (NASA) is working very hard to understand and solve these problems and it is one of the major obstacles that needs to be overcome in order to ensure a safe human trip to Mars by 2030, which has been NASA’s stated goal. Countermeasures, such as negative pressure suits on the torso to pull fluids caudally have already been used in space and other countermeasures such as goggles that could increase the IOP to balance the ICP are under development.
As ophthalmologists, we need to remember that the eye is just an important extension of the body. As we broaden our horizons as a human race, the extremes of physiology will reveal to us the magnificent ways that our bodies work and allow us to ask questions about our basic physiology and seek answers in ways that have been, as of yet, unimaginable.