Assessing Glaucoma Progression
Assessing Glaucoma Progression
Criteria used to define glaucoma progression usually rely on the worsening of functional and/or structural damage.1 However, as yet there are no universally accepted criteria for glaucoma progression. Suitable criteria to define progression may differ depending on thepurpose of the study. As has been suggested in an editorial by Anderson et al., evaluating the course of a disease in an individual patient may be different from identifying small differences in the average course between two or more study groups. It is also different from ascertaining the safety of each individual enrolled in a clinical trial.2 Furthermore, with regard to clinical studies, the progression of one parameter may be more appropriate than others because studies may vary in purpose.2
Criteria for Glaucoma Progression in Randomised Clinical Trials
Previous randomised clinical trials (RCTs) have used different criteria to define glaucoma progression. In the Ocular Hypertension Treatment Study (OHTS)3 and the Early Manifest Glaucoma Trial (EMGT),4 glaucoma progression was defined based on the worsening of both structural and functional damage. With regard to structural damage, in the OHTS progression was defined by generalised or ocalised thinning of the neuroretinal rim compared with baseline. This was determined based on baseline and follow-up stereophotographs assessed by two masked graders.3 In the EMGT, the worsening of structural damage was defined as the progression of optic disc cupping. This was determined based on baseline and follow-up photographs assessed with flicker chronoscopy and side-by-side grading by two masked graders.4 As opposed to the aforementioned studies, the Collaborative Initial Glaucoma Treatment Study (CIGTS)5 and the Advanced Glaucoma Intervention Study (AGIS)6 used only functional damage criteria to define glaucoma progression.
The diversity of criteria for glaucoma progression used in the above RCTs could be related to the fact that the OHTS and the EMGT enrolled subjects with ocular hypertension and earlier stages of glaucoma, respectively, whereas CIGTS and the AGIS included subjects with advanced glaucoma damage. Also, the CIGTS criteria for glaucoma progression were based on visual field only. However, in a recent report by the same study group, baseline and follow-up photographs were assessed by two masked graders to determine the five-year incidence of glaucomatous optic disc progression.7 In this report, optic disc change was recorded as a dichotomous state: no change in cup-to-disc ratio in any meridian versus enlargement of cup-to-disc ratio in any meridian.
Structural and Functional Damage in the Course of Glaucoma
Histological studies suggest that a substantial number of retinal ganglion cells are lost before the development of visual field damage.8,9 It has also been shown that in the earlier stages of glaucoma, optic disc changes are more prominent than visual field defects; however, in the later stages of the disease visual field changes are more prominent compared with morphological changes.10 The fact that structural changes may precede functional changes during the course of glaucoma is further supported by the OHTS, where primary open-angle glaucoma (POAG) development was determined based on changes in the visual field or optic disc as end-points.11 Among the 168 eyes of 152 patients with ocular hypertension that progressed t o POAG in the study, 52% presented with optic disc damage but no visual field defect and 7% presented initially with optic disc damage, followed by visual field defect.
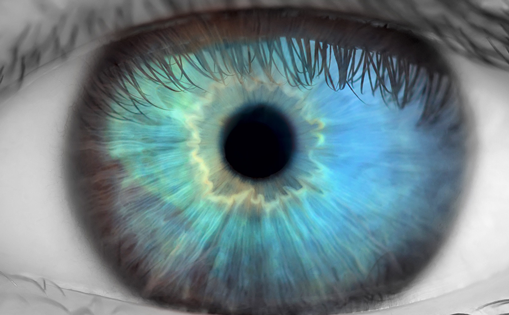
Optic Disc Assessment Is Challenging Even in Diagnosis
Based on all of the above information, observing structural changes is important for determining the progression of glaucoma. However, even in glaucoma diagnosis there are several reasons why optic disc assessment is challenging. The latter requires evaluation of several qualitative and quantitative features. In general, there is a large variability in evaluating the optic disc,12 and this has been observed even among glaucoma experts.13 With regard to specific optic disc features, the interobserver agreement in estimating vertical cup-to-disc ratio has been reported to be moderate (k=0.67) among experts.14 It would therefore be expected to be lower among general ophthalmologists. In addition, in the Thessaloniki Eye Study, glaucoma cases with a relatively small cup-to-disc ratio were more likely to remain undiagnosed.15 Furthermore, clinical assessment of some optic disc features, such as the retinal nerve fibre layer (RNFL), is particularly difficult.16
Structural Changes Associated with Glaucoma Progression
In glaucoma diagnosis, the optic nerve head (ONH) and RNFL can be assessed both qualitatively and quantitatively.1 With regard to qualitative assessment, the neuroretinal rim shape and width, RNFL and disc haemorrhages can be clinically observed. Quantitative assessment involves clinical estimation of the cup-to-disc ratio and rim width, while RNFL thickness cannot be measured clinically. Compared with baseline, changes in all of the aforementioned features can be assessed to determine glaucoma progression. Specifically, progressive diffuse or focal thinning of the neuroretinal rim, new appearance of RNFL, loss or enlargement of a previously detected RNFL and loss and enlargement of cup-to-disc ratio are among the structural criteria for glaucoma progression. The occurrence of optic disc haemorrhages is an additional structural change associated with glaucoma progression.
It is important to note that optic disc haemorrhages are not part of the definition of glaucoma progression. The occurrence of optic disc haemorrhages has been found to be a risk factor for conversion from ocular hypertension to glaucoma by both the OHTS (after five years of follow-up, odds ratio [OR] 3.70, 95% confidence interval [CI] 2.10–6.60).17 Similar results were found in the European Glaucoma Prevention Study (OR 1.97, 95% CI 1.21–3.22)18 after five years of follow-up. In the Collaborative Normal Tension Glaucoma Study, the presence of optic disc haemorrhages was a baseline risk factor for glaucoma progression after five years of follow-up (OR 2.72, 95% CI 1.39–5.32).19 Further to these results, based on a recent EMGT report, after 11 years of follow-up patients with disc haemorrhages had a significantly shorter time to progression (OR 1.03, 95% CI 1.01–1.04) based on clinical data.20
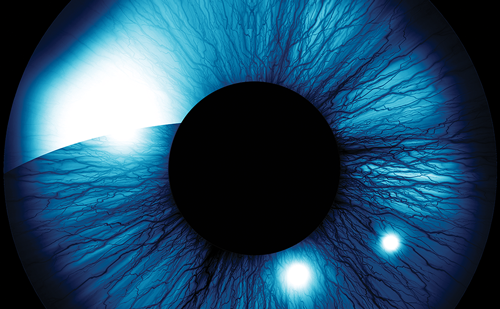
The Use of Photographs in Assessing Structural Changes Associated with Glaucoma Progression
Optic disc stereophotography represents the standard for documentation and monitoring of glaucomatous structural damage, in both clinical practice and research trials.21 However, one should consider that by focusing on optic disc images, true disease progression may be underestimated. Glaucoma progression occurs slowly and changes are often subtle and easily missed. The magnitude of structural changes can be fully appreciated when seeing such changes in a dynamic video format. Furthermore, one should consider that existing data on reproducibility in assessing glaucoma structural changes based on photographs are not encouraging. In the European Glaucoma Prevention Study, where optic disc photographs were graded by senior readers, both the intraobserver and interobserver agreements were moderate (0.79–1.00 and 0.45–0.75, respectively).22 In another study of glaucoma specialists involving 35 pairs of photographs evaluated at least five years apart, the intraobserver and interobserver agreements were even lower (0.55–0.78 and 0.34–0.68, respectively).23 In a more recent study also involving glaucoma specialists, optic disc photographs of 164 eyes were graded after five to 50 months of follow-up.24 The interobserver agreement was found to be extremely low (0.2). In 40% of cases that appeared to have progressed, the optic disc photograph that was assigned ‘worse’ had been taken at the start of the study (graders were masked to chronological sequence).
To date, published data on reproducibility in assessing optic disc photographs refers to glaucoma experts. No studies involving general ophthalmologists have been conducted. An additional limitation related to the use of photographs is that glaucomaprogression is mainly qualitatively evaluated and determined as a dichotomous state: progression versus no progression. Very limited information is provided on the amount of progression. The cupto- disc ratio is the only quantitative measurement when grading optic disc photographs; however, its value with regard to the magnitude of disease progression cannot be fully appreciated unless the reproducibility of measurement and correlation with disease stage are known.
Compared with glaucomatous structural changes, reproducibility in assessing disc haemorrhages seems to be better. In the EMGT, optic disc haemorrhages were assessed based on both ophthalmoscopy and optic disc photographs graded by two masked readers.20 The agreement between the readers on the optic disc photographs was 0.70 (95% CI 0.67– 0.72). The agreement between recordings in clinical forms and on photographs was 0.74 (95% CI 0.66–0.82). In addition, disc haemorrhages were more frequently detected on photographs than with ophthalmoscopy (12.5 versus 9.2%; p<0.0001).
Optic Disc Documentation and Glaucoma Progression
The importance of optic disc documentation in monitoring glaucoma has recently been highlighted in a review by Greenfield and Weinreb.21 Imaging provides a useful record of the appearance of the ONH and RNFL. Simultaneous stereoscopic photography is the preferred method for documenting optic disc appearance, while sequential stereoscopic photography is an acceptable alternative. If colourphotography is not available, annotated detailed drawings can provide documentation. However, both methods are often inaccurate, incomplete and poorly reproducible. In addition, they involve increased variability due to the presence of cataract or a poorlydilated pupil.
Despite the recommendations for imaging of the ONH and RNFL in glaucoma,25 chart reviews from private, community-based ophthalmologists show that there is a lack of compliance with the American Academy of Ophthalmology ONH examination guidelines.26 Among 193 POAG patients followed for ≥2 years in eight private practices in Los Angeles, almost all patients had a photograph or drawing of their optic disc at initial examination. However, at the final follow-up visit, 33.2% had not had an ONH drawing or photograph within two years, while another 37.8% had not had an ONH drawing or photograph since their initial examination. In a more recent chart review study involving 395 patients with POAG in six managed-care plans, only 53% of patients had an ONH photograph or drawing at initial evaluation.27
Summary
Glaucoma progression can be assessed based on the worsening of functional and/or structural damage. Structural changes may be more prominent at earlier stages of glaucoma, while functional changes may be more prominent at more advanced disease stages. Optic disc assessment is challenging, even in glaucoma diagnosis. Structuralchanges suggesting glaucoma progression may involve neuroretinal rim shape and width, RNFL and cup-to-disc ratio. The occurrence of disc haemorrhages is not part of the definition for glaucoma progression but has been recognised as a predictive factor for this.
In both clinical practice and research, colour photography represents the standard for documentation and monitoring of glaucomatous structural damage. However, the limitations related to the use of optic disc photographs to assess glaucoma progression need to be considered. Based on structural changes of the optic disc, glaucoma progression is mainly qualitatively evaluated. However, no information is provided on the amount of progression.
Clinical examination, whether for diagnosis or the detection of progressive change, continues to be limited by the inability of ophthalmologists to accurately and precisely assess the structural appearance of the optic disc. Limitations related to clinical examination could be overcome by the use of imaging technologies.However, specific features of the optic disc, such as disc haemorrhages, can only be assessed clinically.