It is an exciting time in the field of surgical management of glaucoma. The introduction of new devices and procedures that can lower intraocular pressure (IOP) in a safer and less invasive fashion than traditional glaucoma surgery has made it possible to consider a more proactive approach to surgical glaucoma management. This update on innovations in the surgical management of glaucoma will provide an overview of the current and potential future roles of surgery in glaucoma management, discuss the surgical options available for achieving low IOP and highlight the importance of bleb management techniques to improve clinical outcomes in bleb-based surgery.
Surgical interventions in glaucoma management – proactive versus reactive approaches
Ike Ahmed
University of Toronto, Toronto, Canada
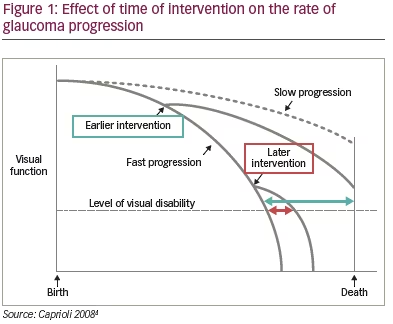
Clinical trials have demonstrated that elevated IOP is associated with the risk of glaucoma progression. In the Early Manifest Glaucoma Trial, patients had a 10% reduced risk of disease progression per mmHg decrease in IOP (hazard ratio [HR] 0.9, 95% confidence interval [CI] 0.86–0.94).1 In the Canadian Glaucoma Study, the risk of disease progression increased by 19% for every mmHg increase in IOP (HR 1.19, 95% CI 1.05–1.36).2 Sustained IOP in the normal range leads to stability of the visual field. It has been reported that eyes with IOP <18 mmHg at every clinic visit over 6 years had almost no change in visual field defect score during follow-up. In contrast, eyes with IOP <18 mmHg at fewer than half of clinic visits had an estimated worsening in visual field defect score of 0.63 (p=0.083).3 The earlier a patient receives intervention to reduce their IOP, the better the outcomes. The impact of an intervention is greater and more sustained if early intervention is provided (Figure 1).4
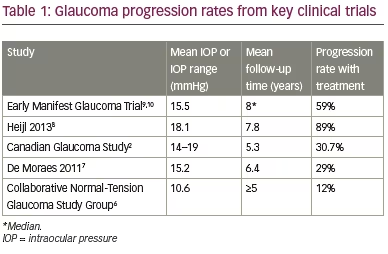
In the traditional treatment paradigm for glaucoma therapy, medication is given in the early stages of the disease and surgery is typically reserved as a ‘last resort’.5 Under this paradigm, the long-term risk of glaucoma progression is still unacceptably high. Several studies show high rates of glaucoma progression despite patients having a mean treated IOP of ≤20 mmHg (Table 1).2,6–10 There is a large variation in the rates of progression in deterioration of the visual field in glaucoma but most patients do progress, at a mean of -0.8 dB/year.8 The probability of glaucoma-related blindness in at least one eye within 20 years of diagnosis with glaucoma is 13.5%,11 and by the time patients die, 42% are blind in at least one eye while 16% are bilaterally blind.12
There are a number of different reasons why people still lose their vision as a result of glaucoma despite advances in diagnosis and treatment. In particular, glaucoma is still under-diagnosed and undertreated and there is still lack of compliance with regard to patients regularly taking their glaucoma medication.13 Reported rates of patients deviating from their prescribed medication regimen are as high as 80% in some studies.14 Data suggest that patients who are poorly adherent tend to experience more severe visual field loss.15 Quality of life (QoL) can also be a significant issue with patients who experience ocular surface disease as a result of using glaucoma medication.16
Interventional glaucoma management encompasses a proactive rather than reactive approach to the disease. It aims to improve patient QoL by preventing blindness, reducing treatment-related QoL issues and improving overall QoL, all while remaining cost effective.17 In terms of IOP reduction, we believe that lower is better, earlier is better and safer is better.2,4 Is it therefore time to change the treatment paradigm for glaucoma and move from a traditional stepwise approach with modest IOP targets to a new, more aggressive approach that aims to achieve a lower IOP earlier? Do we need to reconsider the place of surgery in glaucoma management?17
Glaucoma surgery tends to provide a lower peak IOP with less fluctuation than medication,18 and addresses the problem of compliance. However, despite these benefits we typically leave surgery until very late in the disease, which results in outcomes being less predictable and complications more likely, which in turn, makes us even more reticent to proceed to surgery. Yet, evidence suggests that for patients with advanced glaucoma, surgery should be a first-line treatment option.19 Newer surgical glaucoma devices have allowed us to become more proactive in disease management rather than limiting ourselves to waiting and watching. In our clinic we have used the PRESERFLO™ MicroShunt (Santen, Osaka, Japan), a minimally invasive glaucoma drainage device, over the past 5 years in over 700 eyes.
In an interventional prospective study carried out at our centre, we included 164 consecutive eyes with primary open-angle glaucoma (POAG) or pseudoexfoliative glaucoma without previous glaucoma surgery. The median preoperative IOP was 20 mmHg and patients were taking a median of four medications. Eyes were treated with PRESERFLO™ MicroShunt using 0.2, 0.4 or 0.5 mg/mL mitomycin C applied on sponges for 2–3 minutes. Patients achieved a mean post-operative IOP of around 13.5 mmHg. Rates of post-operative interventions and reoperations were low. Complications were infrequent and not typically vision threatening. Our results compare well with published data on trabeculectomy that show that the proportion of patients achieving success (defined as an IOP of ~17 mmHg or less) can be up to 74% at 2 years with a mean post-operative IOP of ~12 mmHg.20
Beyond surgical IOP reduction, we also need to consider the appearance of the bleb. Thanks to advances in surgical techniques we can now achieve much better bleb formation, considering not only IOP-lowering ability but also morphology, post-operative recovery, refractive impact and long-term outcomes. In my opinion, a posterior bleb is most desirable. In this position the bleb is protected by the upper lid and is less prone to ocular surface trauma, the cells are less metabolically active, the site allows access to more conjunctival lymphatics and there is less attachment of the Tenon’s capsule.
With the PRESERFLO™ MicroShunt, blebs are usually positioned posteriorly and they tend to be fairly diffuse and wide. In my experience, pressure flows are smooth and consistent immediately following surgery with the PRESERFLO™ MicroShunt and it’s a device that requires very little maintenance.
Safer bleb surgery has allowed us to consider more aggressive dosing of mitomycin C to reduce the risk of problems with tissue healing and fibrosis, and newer devices, such as the PRESERFLO™ MicroShunt, allow us to proceed to surgery more rapidly in those patients who we feel would benefit from earlier intervention.
Targeting low intraocular pressure and the roadmap to get there
Ingeborg Stalmans
University Hospitals UZ Leuven, Leuven, Belgium
The PRESERFLO™ MicroShunt was designed in collaboration with ophthalmologists,21–23 and is made of a biostable and biocompatible material, poly(styrene-block-isobutylene-block-styrene), or SIBS.23 SIBS has no degradable bonds and causes minimal foreign-body reaction, inflammation, scarring or capsule formation.24,25 The material is soft25 and extremely flexible,26 conforming to the curvature of the eye, which minimises the risk of erosion.25 It has been used safely in other therapeutic areas. As a cardiac stent coating, it has been tested in clinical trials totalling more than 15 years’ duration and implanted in millions of patients.25,27–29
The PRESERFLO™ MicroShunt is indicated for the reduction of IOP in eyes with POAG where IOP remains uncontrolled while on maximum tolerated medical therapy and/or where glaucoma progression warrants surgery,26 and it received its CE mark in 2012. The device uses the same surgical pathway as trabeculectomy, draining aqueous humour from the anterior chamber to the subconjunctival space and using a subconjunctival/sub-Tenon bleb to bypass the normal drainage pathway (Figure 2).22,25
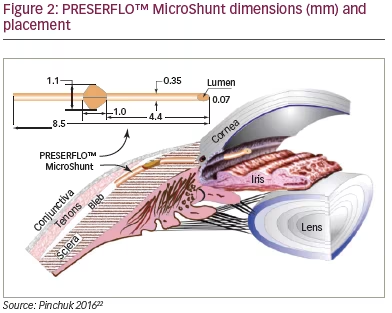
The PRESERFLO™ MicroShunt has an innovative design for implantation into the subconjunctival space,21,22 with ‘wings’ to direct the orientation of the device and prevent migration and leakage around the tube. It also does not have a plate, which permits a less traumatic procedure compared with devices with a plate.22,25 The device is 8.5 mm long overall, with a bevelled end and 70 µm lumen to drain aqueous humour from the anterior chamber through to the bleb whilst providing a careful balance between the prevention of blockage and hypotony and allowing controlled reduction of IOP. The diameter of the tube is just 350 µm, allowing a minimally invasive surgical incision tract to be used.22,25
A comprehensive surgical kit is provided with the PRESERFLO™ MicroShunt, including items such as a scleral marker, slit angled knife, needles, sponges and a marker pen, as well as the device itself.22,26 Minimal extra materials are required; these are standard operating-room tools and consumables such as forceps, scissors and balanced salt solution.
When implanting the PRESERFLO™ MicroShunt, the ideal position for the device is between 11 and 1 o’clock, either superonasal or superotemporal, to stay clear of the extraocular muscles.30 The first step of the implantation procedure (Figure 3) is to inject anaesthetic under the conjunctiva. Anaesthesia can be performed according to the surgeon’s preference and a traction suture can be applied to fix the position of the eye if desired.22,26,31 Next, the conjunctiva is opened at the limbus and Tenon’s capsule is dissected from the sclera using blunt scissors creating a deep and wide conjunctival pocket.
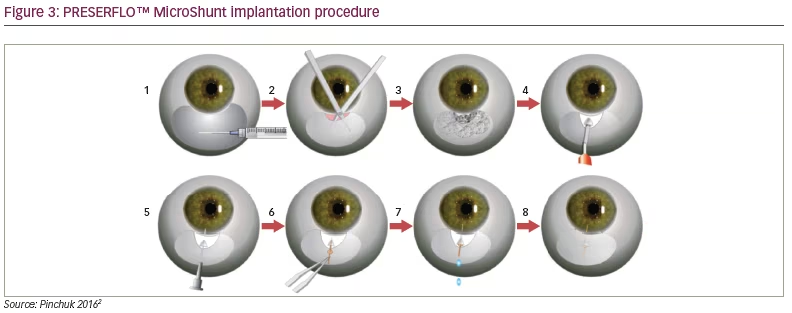
Three sponges saturated with mitomycin C at a concentration of between 0.2 and 0.4 mg/mL are placed in the flap for 2–3 minutes, followed by irrigation with sterile saline solution. A 3-mm mark is
placed from the middle border of the surgical limbus to sclera and the distal part of the tunnel is created using the 1-mm slit angled knife provided. A 25-gauge needle is then advanced through the scleral pocket into the anterior chamber to form a needle tract.22,26,31 The needle is removed and the PRESERFLO™ MicroShunt is inserted through the needle tract with the bevel up until the wings lock into the scleral incision in the wider, distal part of the tunnel and the proximal part of the implant is manoeuvred through the narrower part of the tunnel into the anterior chamber.22,26,31
Flow of aqueous humour from the anterior chamber to the flap should be confirmed by drop observation. Lifting the end of the device away from the conjunctiva might make it easier to observe. If no flow is visible – usually due to the presence of air in the implant – the distal end of the device can be flushed with balanced salt solution using a 23-gauge thin-wall cannula to initiate flow, gentle pressure can be applied to the eye, or the anterior chamber can be filled through paracentesis.22,26,31
Finally, the conjunctiva is closed. The distal end of the PRESERFLO™ MicroShunt should be tucked under Tenon’s capsule, positioned straight and flat on the sclera. Tenon’s capsule is then pulled up and anchored by suture and the conjunctiva sutured closed.22,26,31 Seidel’s test is used to check for leakage from the wound or from conjunctival tears.
Improving odds in bleb-based surgery
Nathan Kerr
Centre for Eye Research Australia, Royal Victorian Eye and Ear Hospital, Melbourne, Victoria, Australia
Significant and sustained reductions in IOP are required to prevent visual field loss in glaucoma and maintain or enhance patient QoL. One of the most important determinants of final IOP and surgical success is wound healing. Like any surgery, bleb-based surgery stimulates a wound healing response, which is characterised by four phases: bleeding, inflammation, proliferation and remodelling (Figure 4).32 By understanding what happens in each of these phases we can target various events in order to increase surgical success. Initially there is bleeding: an injury to blood vessels releasing erythrocytes, leukocytes and platelets. The platelets become activated, releasing cytokines which are potently chemotactic and stimulate the influx of inflammatory cells which triggers the start of the second phase of wound healing, inflammation. There is an influx of macrophages, lymphocytes and neutrophils; these phagocytic cells release proteolytic factors that cause tissue degradation triggering further inflammation.32
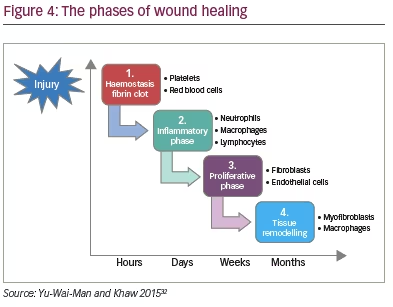
This is followed by the proliferation phase which involves two key components: endothelial cells, responsible for angiogenesis and the formation of new blood vessels, and fibroblasts, one of the most critical cell types involved in the wound healing response, responsible for laying down new collagen and loose connective tissue. This is followed over weeks to months by a remodelling phase, in which the connective tissue is converted into scar tissue.32 This is a critical phase to inhibit so as to increase the success of bleb-based surgery in terms of the efficacy of surgery and the longevity of surgical outcomes.
Glaucoma surgeons have had over 50 years of experience managing blebs with trabeculectomy, and modulating wound healing is something that we are increasingly good at. A number of simple pre-, intra- and post-operative steps have been shown to enhance bleb-based surgery. Studies have shown that treating with glaucoma medications, particularly multiple classes of medications, is associated with the presence of increased numbers of inflammatory cells in the conjunctiva, which is in itself is associated with an increased risk of trabeculectomy failure.7 Pre-operative cessation of glaucoma drops can help to reduce the number and activation of episcleral inflammatory cells,33 which may help to improve surgery outcomes. Another simple thing that can be done in the pre-operative period to reduce the amount of inflammatory cells in the conjunctiva is to treat with topical steroids such as prednisolone acetate four times a day in the week or more prior to surgery.34
Intra-operatively, a number of measures can be taken to improve surgical outcomes. Minimising bleeding is critical,35,36 since reducing the release of blood cells and plasma proteins minimises the trigger for the inflammatory phase. It can be done by using vasoconstrictors such as phenylephrine or adrenaline, by taking care in the handling of the conjunctiva, by implementing cautious haemostasis and (if possible) by withholding anti-coagulants prior to surgery. The recent introduction of minimally invasive surgical techniques and devices, such as the PRESERFLO™ MicroShunt, has meant that glaucoma surgery can now take place with minimal surgical trauma, with no requirement for a scleral flap, iridectomy or releasable sutures.30
The introduction of the use of anti-metabolites was considered a revolution in the success of bleb-based surgery. One of the first to be used in trabeculectomy was 5-fluorouracil (5-FU), a pyrimidine analogue which inhibits incorporation of thymidine into DNA and interferes with RNA synthesis and cell proliferation.37,38 The use of 5-FU has been shown to improve success rates in trabeculectomy up to 3 years after surgery.39 Mitomycin C has been shown to provide better long-term outcomes than 5-FU40 and is probably the most commonly-used anti-metabolite in glaucoma surgery today.
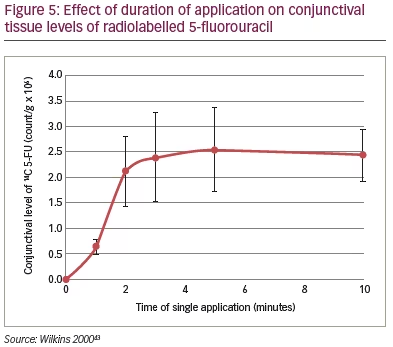
Mitomycin is a potent anti-inflammatory cytotoxic medication which cross-links DNA, inhibits RNA synthesis and reduces cell proliferation.41 To use mitomycin C effectively and safely it is important to consider the concentration or dose of mitomycin C, the time for which it is applied and the method of application. Increased concentrations of mitomycin C result in greater levels of cell death,42 so the appropriate concentration for use in surgery must be tailored to the risk factors of the individual patient. In terms of application time, most anti-metabolites show a rapid increase in conjunctival levels up to around 3 minutes, after which point levels plateau (Figure 5).43 Most surgeons, therefore, adjust the dose of mitomycin C rather than the application time. Finally, the method and area of application of mitomycin C are very important. By treating a broad area of the sclera and sub-Tenon’s the development of a ring of scar tissue can be avoided.44 An advantage of the PRESERFLO™ MicroShunt is that since the conjunctiva is being opened, it is possible to be very accurate with the application of mitomycin C through the placement of sponges.
Post-operatively, inflammation must again be controlled. This can simply be done using topical steroids to reduce the activation of leukocytes, reduce immune activation and minimise vascular permeability.45 Non-steroidal anti-inflammatory agents may also be used; these can modulate wound healing, reduce fibroblast proliferation and reduce fibroblast cell attachment.46 In cases with a more marked fibrotic reaction and suboptimal drainage, bleb function can be restored by mechanically breaking down fibrotic tissue using post-operative needling. Needle revisions can also be augmented with the further application of anti-metabolite.47
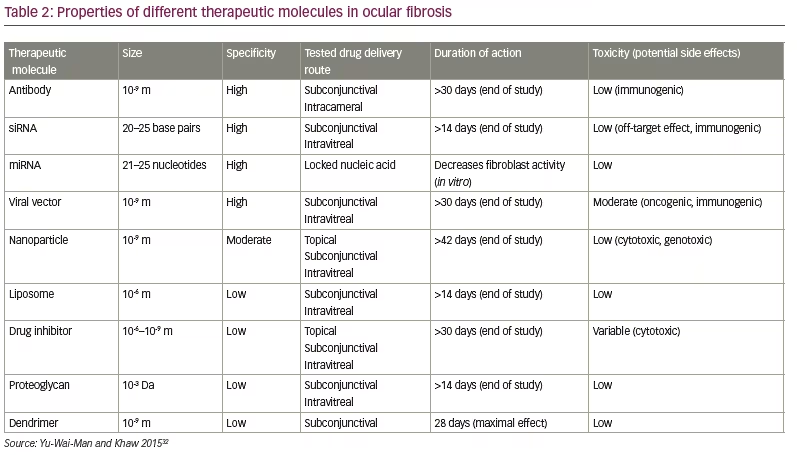
In the future, the success of bleb-based surgery may benefit from a range of new small molecule therapeutics currently under development for the prevention of post-surgical fibrosis, including antibodies, RNAi, gene therapy, nanoparticles, liposomes, dendrimers, proteoglycans and small molecule inhibitors (Table 2).32
Conclusions
Subconjunctival filtration surgery remains the most effective treatment for lowering IOP in patients with glaucoma. With new procedures and devices providing a less invasive approach to glaucoma surgery than traditional trabeculectomy, we may soon see management strategies shift to become more proactive and surgery to be considered earlier. Design features of the PRESERFLO™ MicroShunt that allow it to effectively reduce IOP while reducing procedural risk mean that it is well placed to be part of this paradigm shift. Effective bleb management continues to be important in increasing surgical success, while emerging strategies will ensure continued improvement in surgical outcomes.