Levofloxacin is a later-generation antibacterial agent of the fluoroquinolone class that exhibits a broad spectrum of in vitro activity. It has been demonstrated to be effective in the treatment of a wide range of community- and hospital-associated infections.1 This review presents a microbiological perspective of the use of levofloxacin for topical treatment of bacterial external ocular infections, presenting in vitro, pharmacokinetic and clinical trials data. Levofloxacin eye drops were launched in several European countries in 2002. The widespread use of levofloxacin in ophthalmology can be attributed to its appropriate antibacterial spectrum and good corneal penetration. The main indications for treatment are bacterial blepharitis and conjunctivitis, bacterial keratitis – especially when associated with contact lenses – and endophthalmitis, where it is provided as an additional therapeutic agent. Furthermore, levofloxacin eye drops are used as prophylaxis to reduce the bacterial conjunctival flora prior to intraocular surgery. In a healthy eye the conjunctival bacterial flora primarily consists of Staphylococcus spp. (mainly S. epidermidis), Corynebacterium spp. and, to a lesser degree, Streptococcus spp. and various Gram-negative rods.2 The predominant bacterial organisms isolated from patients with acute bacterial conjunctivitis are S. aureus, S. pneumoniae and Haemophilus influenzae, the latter being frequently recovered from children.3,4 S. aureus is also considered the primary pathogen of chronic blepharoconjunctivitis.
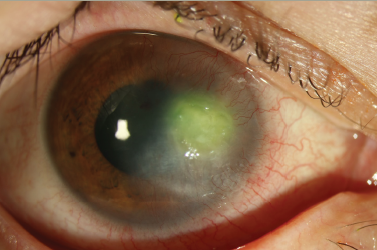
The leading organisms causing bacterial keratitis are Staphylococcus spp., Streptococcus spp., Pseudomonas aeruginosa and enteric Gram-negative rods.5,6 Gram-negative bacilli account for most cases of contact-lensassociated bacterial keratitis.
Pharmacodynamic Properties of Levofloxacin
Levofloxacin is the L-isomer of the racemic drug ofloxacin. The antibacterial activity of ofloxacin resides almost entirely in the L-isomer. Therefore, levofloxacin is, by its nature, twice as active as ofloxacin per unit of mass.7
Mechanism of Action
Like other fluoroquinolones, levofloxacin acts by inhibiting two bacterial enzymes that control the topological state of DNA: DNA gyrase, encoded by the genes gyrA and gyrB, and topoisomerase IV, encoded by the genes parC and parE (grlA and grlB in S. aureus). Both type II DNA topoisomerase enzymes are essential for bacterial growth.8–10 The primary target of levofloxacin in Gram-negative bacteria such as Escherichia coli and Neisseria gonorrhoeae is DNA gyrase, while topoisomerase IV is the primary target in Gram-positive cocci such as S. aureus and S. pneumoniae.7,10 The antimicrobial action of levofloxacin, like that of other fluoroquinolones, is characterised by concentration-dependent bactericidal activity and the ability to induce a post-antibiotic effect against a range of bacteria.1,9
Antibacterial Spectrum
Levofloxacin has broad-spectrum in vitro antibacterial activity against Grampositive and Gram-negative aerobes, as well as so-called ‘atypical’ bacteria such as Chlamydia trachomatis, but has limited activity against anaerobic bacteria.1,9 Figure 1 shows the cumulative distributions of minimum inhibitory concentrations (MICs) of levofloxacin in comparison with ciprofloxacin and moxifloxacin for wild-type populations of four aerobic bacterial pathogens known to cause external ocular infections.11 A microorganism is defined as wild-type for a species by the absence of acquired and mutational resistance mechanisms to the corresponding drug. Clinical MIC breakpoints for levofloxacin against staphylococci, β-haemolytic streptococci, H. influenzae, Moraxella catarrhalis, members of the Enterobacteriaceae family and P. aeruginosa, as suggested by the European Committee on Antimicrobial Susceptibility Testing (EUCAST), are ≤1mg/l and >2mg/l separating susceptible from intermediately susceptible organisms and intermediately susceptible from resistant organisms, respectively, while those against S. pneumoniae are ≤2mg/l and >2mg/l, respectively.12
Levofloxacin displays good activity against wild-type strains of P. aeruginosa (0.063–2mg/l) and is highly active against wild-type strains of H. influenzae (0.008–0.031mg/l), M. catarrhalis (0.016–0.063mg/l) and the Enterobacteriaceae, including Citrobacter spp., Enterobacter spp., E. coli, Klebsiella pneumoniae and Proteus mirabilis (0.016–0.25mg/l). In general, levofloxacin is more active than moxifloxacin (a newer fluoroquinolone), but less active than ciprofloxacin (an earlier fluoroquinolone) against these Gram-negative species. Levofloxacin also shows good in vitro activity against wild-type strains of a range of Gram-positive bacterial species, with MIC values of 0.064–0.5 for S. aureus, 0.5–2mg/l for S. pneumoniae and 0.25–2mg/l for S. pyogenes. In contrast, ciprofloxacin is less active against Gram-positive bacteria, while moxifloxacin has higher in vitro activity.
Resistance
Decreased susceptibility to levofloxacin (and other fluoroquinolones) can develop through two major mechanisms, namely alterations in the drug’s target and alterations that affect the intracellular concentration of the drug. Target-site alterations are linked to mutations in the quinolone-resistancedetermining region (QRDR) of the gyrA and parC genes.7,10 Such mutations usually result from errors during chromosome replication, but can also be acquired via horizontal gene transfer, which has been observed in S. pneumoniae and viridans group streptococci.13,14 A high level of resistance to levofloxacin requires mutations in more than one gene.15
The second main mechanism of resistance, which is associated with a decrease in the intracellular concentration, results from changes in the outer membrane of bacteria (limited to Gram-negative bacteria) and/or drug efflux.7 Recently, plasmid-mediated quinolone resistance genes (qnr) have been described in E. coli and other Enterobacteriaceae species.16 The Qnr proteins are capable of protecting DNA gyrase from quinolones. Increasing levels of resistance to fluoroquinolones have been reported worldwide over the past 10–15 years. For example, among German E. coli isolates recovered in the surveillance studies conducted by the Paul Ehrlich Society (PEG) between 1995 and 2004, resistance to fluoroquinolones (ciprofloxacin, levofloxacin) increased from 5 to 22%.17 However, the data from the PEG studies were mainly recorded at tertiary care hospitals with a high proportion of nosocomial pathogens. Therefore, the rates of resistance found here may not be interpreted as representative of the outpatient sector.
Prevalence of Resistance Among Ocular Pathogenic Bacteria
Staphylococcus aureus: The rates of susceptibility and resistance to the fluoroquinolones (including levofloxacin) often resemble those of methicillinsusceptible S. aureus (MSSA) and methicillin-resistant S. aureus (MRSA).
Most of the MSSA are susceptible to fluoroquinolones, while the majority of MRSA are resistant. Data from Ocular TRUST 1, a prospective multicentre surveillance study conducted in the US between October 2005 and June 2006, show that the rates of levofloxacin resistance were 18.9 and 78.8% among the MSSA isolates (n=164) and MRSA isolates (n=33), respectively.18 According to data from a German prospective surveillance study conducted in 2004 evaluating 436 S. aureus isolates recovered from patients with external ocular infections in 35 laboratories, the level of resistance to levofloxacin was 5% among the MSSA (n=380) and 53.6% among the MRSA (n=56).19
Streptococcus pneumoniae: The emergence of fluoroquinolone-resistant strains of S. pneumoniae has been reported in recent years in some parts of the world, in particular in South-east Asia.20,21 However, the overall incidence of fluoroquinolone resistance among pneumococci seems to remain low. All 49 isolates collected during Ocular TRUST 1 were levofloxacin-susceptible. In addition, all archived 760 ocular isolates collected during the longitudinal TRUST surveillance programme between 1996 and 2006 were susceptible to levofloxacin, except one.18 The German surveillance study found that 184/187 (98.4%) were susceptible.19
Haemophilus influenzae: All isolates collected during Ocular TRUST 1 (n=32) were susceptible to levofloxacin, as were 355/356 (99.7%) of the archived isolates from TRUST, regardless of β-lactamase production.18 The German surveillance study found that all 164 isolates examined showed susceptibility to levofloxacin.19
Other ocular pathogens: Data from the German resistance surveillance study for ocular organisms indicated that none of the 46 E. coli isolates and 6/45 (13.3%) of the P. aeruginosa isolates were resistant to levofloxacin,19 five of which were isolated from hospitalised patients.
Pharmacokinetic and Toxicological Properties
After a single drop of 0.5% levofloxacin ophthalmic solution applied to each eye of healthy volunteers, drug concentrations in the tear fluid remained above 2mg/l for at least six hours.22 Following topical administration, the drug has also been demonstrated to effectively penetrate the cornea, and if the drug is frequently given over one hour, concentrations achieved in the anterior chamber of the eye were above the MICs of most ocular bacterial pathogens.23–25 When combined with orally administered levofloxacin, adequate drug levels were also achieved in the vitreous cavity of the eye.>sup>26 Topically applied fluoroquinolones have been considered to be more toxic to the corneal epithelium than other antibiotic agents.27,28 However, in a recently published study levofloxacin did not negatively influence epithelial wound healing.29 Moreover, levofloxacin was shown to be less cytotoxic on human corneal keratocytes and epithelial cells than other fluoroquinolones, including gatifloxacin, moxifloxacin, ciprofloxacin and ofloxacin.30
Pharmacokinetic/Pharmacodynamic Relationships
The ratio between the 24-hour area under the serum concentration curve and MIC (AUC24h/MIC) and the peak concentration/MIC (Cmax/MIC) for unbound drug are thought to be predictors of clinical and bacteriological efficacy.31 However, the magnitude of the pharmacokinetic/pharmacodynamic (PK/PD) index needed seems to vary according to the type of quinolone, bacterial species and immune status. A Cmax/MIC ratio of >10 and an AUC24h/MIC ratio of 100–125 has been reported to provide maximum bacterial eradication and to prevent resistance in critically ill patients with nosocomial lower respiratory tract infections caused by Gram-negative bacteria such as P. aeruginosa.32,33 However, in outpatients with community-acquired respiratory tract infections such as acute exacerbations of chronic bronchitis and community-acquired pneumonia caused by S. pneumoniae, AUC24h/MIC ratios of about ≥25 are predictive for bacterial eradication.10,34 Based on the tear concentrations measured in the healthy volunteer study by Raizman et al.,22 the calculated AUC over six hours after the instillation of a single dose (one drop) of 0.5% levofloxacin ophthalmic solution was more than two-fold higher than the AUC24h after a single oral or intravenous administration of 750mg levofloxacin. In clinical practice the AUC should even be higher, as patients would receive multiple doses per day. These data indicate that a 0.5% levofloxacin ophthalmic solution is effective in the treatment of external ocular infections against target pathogens.
Clinical Trials
A topical ophthalmic solution of 0.5% levofloxacin was effective in bacterial conjunctivitis and keratitis.35–39 In a study by Yactayo-Miranda et al., so far published only as a poster, 0.5% levofloxacin eye drops were also effective in the treatment of chronic bacterial blepharoconjunctivits.40 More recently, there has been increasing interest in the use of levofloxacin as a prophylactic agent in intraocular surgery. Because of its broad spectrum of antibacterial activity and high corneal permeability, levofloxacin appears to be a suitable agent for this purpose as it has been shown to reduce the bacterial conjunctival load, being the main source of bacteria causing post-operative infections, and to achieve drug levels inside the eye that are capable of preventing infection in cases of contamination.23–25,41 Levofloxacin proved to be effective as prophylaxis in intraocular surgery and acted synergistically when combined with the standard conjunctival povidone–iodine irrigation.42,43 Recently, 0.5% levofloxacin eye drops were evaluated for the prevention of post-cataract surgery intraocular infection. In this large-scale European multicentre trial, the difference in the rates of post-operative infections between levofloxacin and placebo did not reach statistical significance, although the dosing regimen was met with some criticism (low dose and late time-point of post-operative prophylactic treatment), and an unexpected high incidence of post-operative infections was observed in the placebo arm.44
Conclusions
Despite the long-term extensive use of fluoroquinolones for the treatment of local and systemic infections, levofloxacin-resistant ocular isolates of S. pneumoniae and H. influenzae remain uncommon. Also, based on the data of the German surveillance study, the treatment of superficial ocular infections caused by E. coli and P. aeruginosa with levofloxacin still have a high likelihood of success. In contrast, levofloxacin, like other fluoroquinolones, is not indicated if MRSA is suspected as a pathogen. Due to its high corneal penetration, levofloxacin represents one of the most valuable antibacterial agents for topical use in ophthalmology, especially for the treatment of fulminant bacterial keratitis. However, its role as a prophylactic regimen in ocular surgery needs to be further elucidated.