Optical coherence tomography (OCT) is a noninvasive, objective optical modality providing cross-sectional images of in vivo tissue at a micrometer resolution scale.1 Since the first reports of its use in ophthalmology by Puliafito and Fujimoto in 1991,1 OCT has been widely used and it is now one of the most useful devices in ophthalmic clinical practice.
Optical coherence tomography (OCT) is a noninvasive, objective optical modality providing cross-sectional images of in vivo tissue at a micrometer resolution scale.1 Since the first reports of its use in ophthalmology by Puliafito and Fujimoto in 1991,1 OCT has been widely used and it is now one of the most useful devices in ophthalmic clinical practice.
The first OCT machine on the market was manufactured by Carl Zeiss Meditec in 1995; however, only in the past 10 years has OCT become largely available commercially. OCT technology was first applied to the retina, with clinical applications of OCT to retinal disease increasing over the past decade; OCT has overcome the adverse effects associated with fluorescein angiograms and, in many cases, is more informative.
OCT of the anterior segment is an evolution of the retinal OCT. It uses a longer wavelength (1,310 nm) than the retinal OCT (820 nm), which enables greater penetration through tissues that scatter light, such as sclera and limbus. Anterior OCT can visualise the corneal structure, the iridocorneal angle and the anterior lens. Imaging depth is limited to the pigment epithelium of the iris, which acts as a barrier to this optical method.
Briefly, in the OCT machine, an infrared beam is directed at a sample and the delay of the reflected light is measured. OCT measures the wave delay by comparing the sample reflection with a reference reflection in an interferometer. OCT has changed considerably in recent years, with the incorporation of spectral domain (SD) technology, which offers significant advantages over the traditional time domain (TD) OCT. Owing to their high frame transfer rate and fast Fourier transform algorithm, these recently introduced devices can perform up to 27,000 A-scans per second with a depth resolution of approximately 5 μm.2,3
Until the development of Fourier domain OCT techniques, including SD-OCT, OCT was a two-dimensional (2D) examination modality. The new generation SD-OCT offers a faster acquisition speed and an increased depth resolution compared with TD-OCT. In addition, it enables the three-dimensional (3D) in vivo examination of eyes.4,5
RTVue (Optovue Inc, Fremont, CA) is one of the commercially available instruments using SD-OCT technology to obtain cross-sectional and 3D images of both the posterior and anterior segments. It uses a scanning laser diode to emit a scan beam with a wavelength of 840 ± 10 nm. Unlike TD-OCT, RTVue uses a stationary reference mirror, and the OCT signal is acquired using a spectrometer as a detector. It offers a higher resolution than does TD-OCT, providing a significant reduction in motion artefacts and an increased signal:noise ratio compared with TD-OCT. RTVue can also perform up to 26,000 A-scans per second with a depth resolution of approximately 5 μm. For corneal and anterior segment imaging, an adaptor lens is mounted on the front objective lens.
The use of OCT is well established in adult patients for the management of retina and optic nerve head (ONH) disease. Recently, OCT has been widely used in graft assessment after corneal surgery.6–8 By contrast, the clinical application of OCT in paediatric patients is poorly studied.
Currently, interest in the use of OCT in paediatric patients is mainly focused on retinal disease,9 with recently published papers reporting the macular changes in patients with ocular albinism10 and the OCT macular appearance of preterm children with and without retinopathy of prematurity.11
In this paper, we report our experience using SD-OCT with paediatric patients affected by congenital cataract and aniridia. To the best of our knowledge, this is the first report of this use of SD-OCT.
Aniridia
Congenital aniridia is a rare ocular disease affecting the development of multiple ocular structures. It is genetically determined by a mutation in the paired box 6 (PAX6) gene located on chromosome 11p13.12–14
The name of the condition comes from iris hypoplasia, the most common sign of the disease. Clinical findings arising from various mutations in PAX6 are corneal opacities, cataract, and foveal and optic nerve hypoplasia (ONH). Aniridia can often be complicated by glaucoma. Patients with aniridia have severe visual impairment and foveal hypoplasia is usually the leading cause of poor vision in such patients.15
Congenital Cataracts
Any opacity of the lens diagnosed at birth is considered a congenital cataract. Unilateral congenital cataracts are generally not associated with systemic disease and are rarely inherited; in most cases, the cause is idiopathic.
The cause of bilateral congenital cataract is also usually idiopathic. One-third of cases are reported to be hereditary, with or without a systemic disease.16 Bilateral cataracts associated with systemic diseases require a full metabolic, infectious, systemic and genetic workup. The most common conditions associated with bilateral cataracts are metabolic disorders, such as galactosaemia and hypocalcaemia.17
Other conditions associated with bilateral cataracts are trisomy (e.g. Down’s, Edward’s and Patau syndromes), myotonic dystrophy, infectious diseases (e.g. toxoplasmosis, rubella, cytomegalovirus and herpes simplex) and prematurity. There are several types of congenital cataract. Nuclear cataracts are usually present at birth and are nonprogressive. This opacity is bilateral in approximately 80 % of cases. Posterior unilateral cataracts in infants and children are commonly associated with persistent foetal vasculature and the involved eye is generally microphthalmic. In addition, posterior cataracts can be associated with posterior lentiglobus. Lamellar cataracts involve the lamellae surrounding the foetal nucleus peripheral to the Y sutures. This cataract is progressive and usually develops after fixation is established. Lamellar cataracts are bilateral and commonly have an autosomal dominant pattern of inheritance. Other morphological types of congenital cataract are sutural cataracts and anterior polar cataracts, which usually do not progress.18 In children with congenital cataracts, visual loss and development of amblyopia depend on the size and location of the cataract. Dense central opacities involving the visual axis and >3.0 mm in diameter are generally considered visually significant and usually need surgical removal.
Opacification of the visual axis caused by posterior capsule opacity is the most common complication after cataract surgery in children19 and nearly 80 % of eyes with an intact posterior capsule develop posterior capsule opacity.20 To diminish the rate of opacification in the postoperative period, a posterior capsulorhexis and anterior vitrectomy at surgery is generally performed, particularly in preschool children. The most sight-threatening complication is the development of a secondary glaucoma. Aphakic or pseudophakic glaucoma can occur from months to decades after cataract surgery in children.21 The incidence of glaucoma seems to depend on the time of surgery, with the highest incidence in patients younger than two months and a lower incidence when surgery is performed in children older than one year.22 To rule out the development of glaucoma intraocular pressure (IOP), corneal diameter and axial length should be regularly measured and the optic disc examined during follow-up visits. The IOP and optic nerve should be controlled throughout the life of every child treated for congenital cataract.
Methods
Aniridia
The inclusion criteria for this study were paediatric patients (<14 years) with aniridia older than three years and cooperative for ophthalmic examination and OCT. In total, 12 consecutive patients with aniridia referred to the San Giuseppe University Eye Clinic from November 2010 to October 2011 were included in this report. Children underwent ophthalmic exam and SD-OCT. The best-corrected visual acuity was recorded in cooperative patients. The presence of keratopaty, and cataract and foveal hypoplasia were investigated by both slit-lamp exam and OCT. The depth of the angle and the ONH appearance were also investigated to evaluate the presence of angle closure or open angle glaucoma.
Congenital Cataracts
Inclusion criteria for this study were paediatric patients (<14 years) with congenital cataracts older than three years and cooperative for ophthalmic examination and OCT. These patients either had undiagnosed congenital cataracts at birth or progressive congenital cataracts that were clinically unremarkable at birth. In total, five consecutive patients referred to the San Giuseppe University Eye Clinic from November 2010 to October 2011 fulfilled the inclusion criteria and were included in this report. Before surgery, children underwent ophthalmic exam and SD-OCT. The best-corrected visual acuity was recorded in cooperative patients.
One day, one week, one, two, three and six months after surgery, children underwent SD-OCT. The following parameters were assessed by OCT: (before surgery) the type of lens opacity; (after surgery) the intraocular lens (IOL) position in the bag, the corneal incision healing and the presence of posterior capsule opacity (PCO).
Reproducibility and Quality of Optical Coherence Tomography Measurements
All OCT examinations were performed by a single expert operator (MS). The intraobserver variability (i.e. repeatability) for the posterior capsule and cornea thickness analyses was calculated using the intraclass correlation coefficient (ICC). Only images with a scan score index (SSI) >30 were included in the analysis. In cases where the SSI was <30, the measurement was repeated.
Results
Aniridia
In total, 24 eyes of 12 consecutive patients were examined. The mean age was 5.5 ± 3.2 years (range, 3.4–9.8 years). Best-corrected visual acuity was assessed in seven patients (58.3 %) and in six eyes ranged from 20/100 to 20/200, in four eyes from 20/60 to 20/100, in two eyes was 20/60 and in two eyes 20/40.
Keratopaty
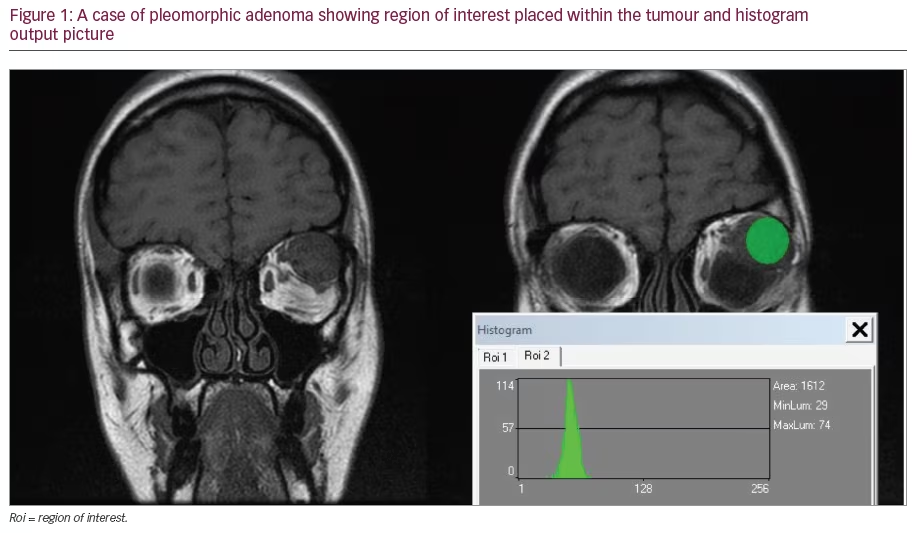
Keratopaty was observed in 14 eyes (58 %) by slit-lamp exam, whereas various degrees of corneal opacity were found by SD-OCT in 18 eyes (72 %) (see Figure 1A). In four eyes, subtle corneal involvement was not observed by a slit-lamp exam, but was visualised by OCT.
The corneal involvement was consistent with band keratopaty in eight eyes (33.3 %); 11 eyes 45.8 %) showed various degrees of subepithelial fibrosis; and five eyes (20.8 %) were affected by corneal opacity with neovascularisation.
Cataracts
Of the 24 enrolled eyes, 16 (66.6 %) had various degree of lens involvement (see Figure 1B). Posterior subcapsular lens opacity was the most common type of cataract. In 10 eyes (41.6 %), cataracts were considered clinically relevant and phacoemulsification with IOL implant was scheduled. OCT was able to visualise the cataract and the IOL position in the bag after surgery.
Fovea Hypoplasia
Fovea hypoplasia was detected in 15 eyes (62.5 %) by SD-OCT as loss of normal foveal architecture and absence of normal foveal depression (see Figure 1C). Foveal hypoplasia, defined as the absence of a foveal reflex, was found in nine eyes (37.5 %) by slit-lamp exam.
Glaucoma
In total, 15 eyes (62.5 %) were affected by glaucoma; 11 eyes had previous angle surgery; six eyes had previous trabeculectomy; 10 eyes were under topical medication for glaucoma; and three eyes had untreated, newly detected glaucoma.
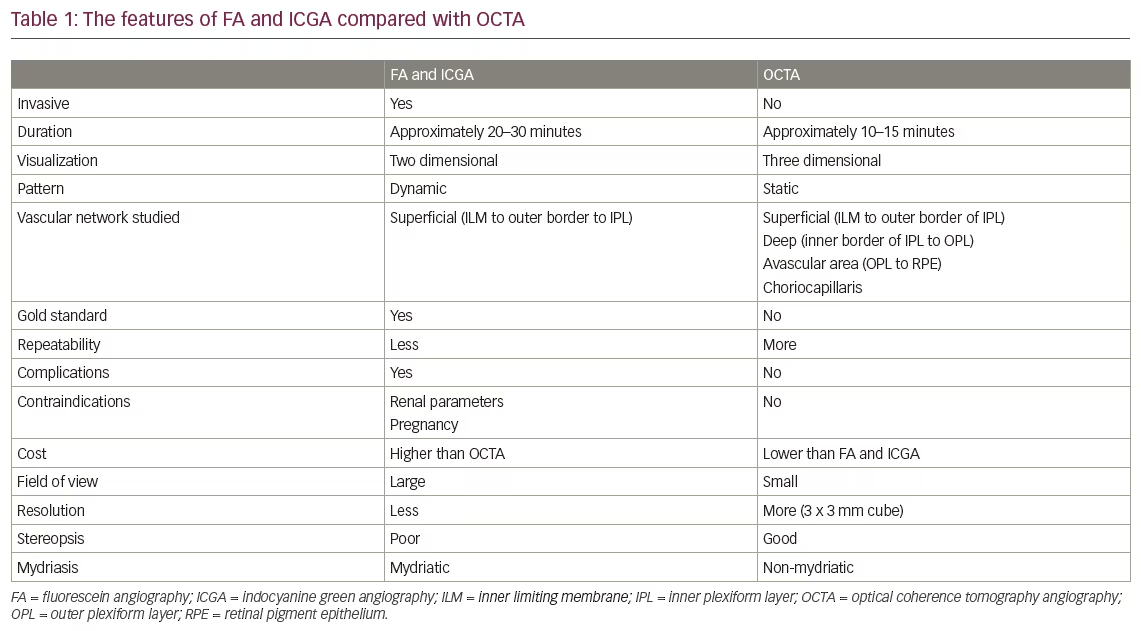
It was possible to use OCT to investigate the iris hypoplasia and angle depth (see Figure 1D). The angle was open in all patients where glaucoma was associated with aniridia. The optic nerve head was assessed by ophthalmic and OCT exam (see Figure 1E). Both examinations revealed optic nerve changes consistent with glaucoma in 15 eyes (62.5 %). Aniridia-associated findings are summarised in Table 1.
Congenital Cataracts
In total, seven eyes of five consecutive patients were examined. The mean age of the patients was 4.5 ± 2.1 years (range, three to seven years).
It was possible to use OCT to visualise the different types of lens involvement in the paediatric patients enrolled in this study (see Figure 2A). On the basis of the OCT images, we categorised congenital cataracts into five groups: anterior polar cataract (2); anterior sub capsular cataract (1); laminar cataract (1); posterior cortical cataract (2); and posterior sub capsular cataract (1).
After careful examination of two eyes (one with a mild anterior polar cataract and one with a posterior subcapsular cataract), the cataracts were evaluated as clinically unremarkable and surgery was not considered. Five eyes were included in the analysis.
After surgery, the IOL was easily visualised in the bag by OCT and the relationship between the IOL and the bag, and the IOL and the iris was recorded. In one case, the OCT exam revealed a slightly tilted IOL because of residual cortex under the IOL plate. However, surgical revision was not necessary (see Figure 2B,C).
The posterior capsule was well visualised in all patients during the follow-up and the posterior capsule thickness was recorded. The ICC for the posterior capsule thickness evaluation was 0.89.
The thickness of the normal, clear posterior capsule on slit-lamp exam was found by OCT to range from 12 to 18 μm. Slit-lamp exam revealed a mild PCO in two cases. Posterior capsule thickness ranged from 28 to 35 μm. A clinically relevant PCO was found in one eye. The thickness of the posterior capsule ranged from 47 to 77 μm. This case required Nd:YAG laser posterior capsulotomy. On the basis on these findings, we suggested a PCO staging using the OCT measurements of the posterior capsule thickness, with the normal, clear posterior capsule ranging from 12 to 20 μm, the incipient PCO ranging from 25 to 45 μm and with the PCO having a posterior capsule thickness >45 μm (see Figure 3).
Corneal healing after surgery was followed by OCT to evaluate the thickness and architectural changes of the cornea incision site during the follow-up. The ICC for corneal thickness evaluation was 0.82. The mean corneal incision site thickness was 807.4 ± 18.6 μm at baseline, 990.1 ± 36.8 μm (P <0.001) one month and 812.8 ± 21.6 μm (P = 0.51) six months after surgery.
Corneal incision healing can be visualised as a reflective line along the incision site. Architectural changes of the corneal incision site seem to suggest stable healing after the first postoperative month, with a mildly reflective line visualised by OCT. At the end of the follow-up, corneal incision healing detected by OCT seemed to be complete and a highly reflective line could be detected along the incision site (see Figure 4).
Discussion
Knowledge of the repeatability and quality of OCT measurements is important, particularly when dealing with children. According to guidelines proposed by Landis and Koch,23 the agreement was very good for both the posterior capsule and the cornea thickness evaluation. Patients enrolled in the study were older than three years of age. At this age, children are generally able to cooperate effectively. All the enrolled patients, according to the inclusion criteria, were able to cooperate for the OCT exam.
In our series of patients with aniridia, the most common ocular anomaly was the keratopaty affecting 72 % of the patients. The keratopaty in aniridia seems to be the result of a limbal stem cell deficiency.24,25 Corneal involvement ranged from peripheral pannus with a relatively clear central cornea to various degrees of subepithelial fibrosis and stromal haze. With age, neovascularisation might gradually advance into the central cornea until the entire cornea is involved. Corneal involvement was better assessed by OCT in our study.
Retinal involvement was shown to be underestimated by slit-lamp exam, with foveal hypoplasia detected in nine eyes by slit lamp compared with 15 eyes by SD-OCT. The fast acquisition speed of SD-OCT enabled useful information to be obtained during only a few seconds; the ability to analyse images after the examination allowed to the presence of keratopathy and foveal hypoplasia to be better quantified.
Glaucoma is thought to be related to progressive circumferential changes in the angle, along with the gradual forward migration of abnormal iris tissue on the posterior trabecular meshwork.26 Glaucoma development significantly affects the long-term visual outcome in patients with aniridia. Children with aniridia should therefore be kept under close surveillance for the development of glaucoma. Increased central corneal thickness leads to a significant overestimation of the IOP in patients with congenital aniridia and perimetric analysis might not always be successful in children.
Therefore, careful and regular examination of the optic disc is important for the detection of glaucoma in patients with aniridia. In our study, OCT was able to detect objectively the morphological changes of the optic nerve as well as the depth of the angle. OCT was also able to visualise the position of the IOL after surgery. This is a new potential target for OCT. It has been reported that aniridia has a profibrotic nature.27 Fibrosis syndrome in aniridia is characterised by the development of a progressive fibrosis involving the cornea and IOL after intraocular surgery. The postulated mechanism of the formation of this fibrotic material is the proximity or touching of IOL on immature vessels in the rudimentary iris, subclinical chronic inflammation and the unique vulnerability to progressive fibrosis caused by PAX6 mutations. Patients with aniridia with a history of surgery, such as for IOLs and tube shunts, should therefore be monitored for aniridic fibrosis syndrome. OCT can also be used to determine the position of the IOL and the relationship between the IOL and the hypoplastic iris, providing information that is useful for visualising the correct position of the IOL and for monitoring the development of aniridic fibrosis syndrome more closely (see Figure 2C).
In children with congenital cataracts, PCO is the most common postoperative complication affecting vision, even after uneventful surgery. We used OCT to quantify objectively the posterior capsule thickness after cataract surgery and we found that a thickness >45 μm was consistent with clinically significant PCO. In our experience, in children with poor cooperation, the possibility of obtaining a posterior capsule measurement by OCT can provide data that is more informative than that provided by slit-lamp examination, because OCT enables physician to take the acquisition in a couple of seconds and to analyse the images after the exam.
Corneal incision healing is an important consideration when patients are children, because of the high risk of trauma, especially in preschool children. The highly oedematous cornea, as visualised by SD-OCT at the site of incision, is likely to be unstable and at risk of wound opening, particularly during the first week after surgery. Throughout the first month after surgery, we were able to follow the healing as a reflective line at the incision site. This finding seemed to be consistent with more stable healing after the first postoperative month, with complete healing six months after surgery. This result suggests that parents should be particularly careful during the first month after surgery with the activities that their children undertake.
Conclusion
The indications of OCT have been increasing during the past 15 years, from retina, to ONH, angle and cornea. Paediatric ophthalmology is a challenging niche of the ophthalmic clinical practice and pathologies, such as cataract, glaucoma or corneal diseases, are far to have the same pathophysiology and management than in adults. The major advantages of the newer, spectral domain devices are their noncontact nature, high acquisition speeds, the range of quantitative and qualitative information they provide, the ability to obtain a 3D in vivo examination of human eyes, and their safety, even in a paediatric population. With the introduction of new generation, high-speed OCT, paediatric ophthalmology is likely to become an interesting new field for OCT application. The shape and the dimension of the cataract, the IOL position, the posterior capsular bag and the incision healing are potential new targets for OCT. On the basis of our results, it seems that, in children with aniridia and congenital cataracts, OCT can provide clinically relevant information. In conclusion, therefore, OCT is a promising tool to supplement clinical practice and for ophthalmic research, even in paediatric ophthalmology. ■