Anterior uveitis denotes intraocular inflammation that involves the iris (iritis), anterior part of the ciliary body (anterior cyclitis), or both (iridocyclitis). Primary site of inflammation, as determined clinically, is the anterior chamber and/or anterior vitreous.1 The standardization of uveitis nomenclature (SUN) working group has categorized uveitis according to the onset, duration, and course of the disease.1 Anterior uveitis can be of an acute or insidious onset. The duration of anterior uveitis can be limited (less than or equal to three months) or persistent (more than three months). Anterior uveitis is also classified based on the disease course: It is classified as acute anterior uveitis when there is an episode of sudden onset and limited duration; recurrent anterior uveitis when repeated episodes occur separated by periods of inactivity for at least three months without treatment; and chronic anterior uveitis when it persists and relapses in less than three months after discontinuing treatment. Anterior uveitis may also be classified as granulomatous or non-granulomatous according to its clinical appearance, and infectious or non-infectious according to its etiology. A clear classificaton of uveitis helps clinician in performing investigations and laboratory tests. Anterior uveitis can be associated with various systemic diseases and further systemic physical examination and investigations should be carried out when required. With a systematic approach, including detailed history, ocular examination and ancillary investigations, a diagnosis can be established in up to 70 % of cases.2
Although causes of uveitis differ among the various regions of the world, anterior uveitis is the most common form of intraocular inflammation at uveitis centers worldwide.3–6 Anterior uveitis is usually the most easily managed form of uveitis. However, in some cases it can lead to sightthreatening and serious complicatons such as glaucoma, cataract, and cystoid macular edema. Complications can be prevented or managed earlier, if anterior uveitis is promptly diagnosed and appropriately treated.
Symptoms of Anterior Uveitis
As anterior uveitis can present with an acute, chronic, or recurrent form, the severity of symptoms ranges from no symptoms in chronic disease to very severe symptoms in acute uveitis. Patients with insidious-onset chronic anterior uveitis do not have symptoms until the development of complications that cause blurred vision. Young children with chronic anterior uveitis are typically asymptomatic.7 By contrast, patients with acute anterior uveitis associated with the HLA-B27 antigen are severely symptomatic and start feeling a dull ocular pain even before any evidence of an acute attack can be detected on clinical examination. Symptoms of acute anterior uveitis include pain, photophobia, redness, tearing, blurred vision and floaters.
Pain
The pain of anterior uveitis usually results from acute inflammaton of the iris and ciliary body and is most severe when the patient fixates at a near object, especially a light source. Ciliary and iris sphincter muscle spasm can cause varying degrees of pain that may be described as a dull aching type of pain or a throbbing sensation localized to the eye, but may also be a referred pain that seems to radiate over a larger area served by the trigeminal nerve. In contrast to the ocular pain associated with scleritis or papillitis, a nocturnal pain is not specifically reported and pain does not increase with eye movements.
Photophobia
Photophobia is usually caused by ciliary muscle spasm but can also be associated with pupillary muscle involvement or corneal epithelial edema.
Tearing
Tearing is seen as a result of trigeminal nerve irritation.
Floaters and Blurred Vision
Inflammatory cells, fibrin, or opacities in the anterior vitreous can cause floaters. Corneal edema, occlusion of the pupillary area with a dense fibrin clot, opacities in the anterior vitreous, ciliary spasm, macular edema, and secondary cataract can cause blurred vision in anterior uveitis.
Clinical Signs of Anterior Uveitis
Ciliary Injection
In iritis or iridocyclitis the enlargement of episcleral vessels around the limbus is seen in dark red color. There may also be diffuse conjestion of the bulbar conjunctival vessels; however, circumcorneal injection is more prominent.
Keratic Precipitates
Keratic precipitates (KPs) are inflammatory cellular deposits on the corneal endothelium. The morphology and distribution of KPs help the differential diagnosis of anterior uveitis.2 The morphology of KPs may change from dust-like particles to large deposits. Aqueous humor circulation in the anterior chamber originates from tempature differences. Aqueous cells move upward with warming up of the aqueous on the surface of the iris and move downward with cooling down of the aqueous on the endothelial surface of the cornea.8 Due tothis circulation pattern and gravity, inflammatory cells usually accumulate on the lower half of the cornea often in a base-down triangle configuration. The well-recognized exceptions to this distribution include Fuchs uveitis where KPs are evenly distributed all over the corneal endothelium and herpetic uveitis where KPs are accumulated in a circular pattern on the surface of central or paracentral corneal endothelium.9 Neutrophils and lympho-plasmocytic cells accumulating on the endothelium may give rise to endothelial dusting in eyes with high-grade anterior chamber cells in acute or chronic nongranulomatous anterior uveitis.10 Sometimes fine dust-like KPs may be seen in a perpendicular linear pattern. Presence of any KP morphology larger than dust designates granulomatous inflammation.
Granulomatous KPs may be microgranulomatous, medium sized, or large. Endothelial deposits of lymphocytes, macrophages, and epithelioid cells forming large granulomatous KPs with a greasy apperance are defined as ‘mutton fat’ KPs. They are typically seen in granulomatous diseases such as sarcoid uveitis.11 Large flat KPs of grayish or rusty color are typical of acute herpetic anterior uveitis,12 but may also be seen in other infectious entities. Microgranulomatous or medium sized KPs may form in eyes with low-grade chronic anterior uveitis. In cytomegalovirus-associated anterior uveitis, medium-sized granulomatous KPs may be surrounded by a translucent halo and sometimes accompanied by a spot of pigment.13,14 According to the type and stage of inflammatory process, a mixture of fine and granulomatous KPs may be seen and KP morphology may change with treatment. Endothelial dusting may disappear without any trace or with only sparse fine pigment deposits. Large granulomatous KPs may become smaller, less greasy, and then become pigmented or completely disappear. ‘Foot prints’ of granulomatous KPs may be seen in some cases following complete resolution of inflammation. Fine stellate KPs and granulomatous KPs with stellate extensions are typical of Fuchs uveitis and are usually stable over the course of the disease.2,9,15,16 Fine pigment precipitates on the corneal endothelium seen after resolution of anterior uveitis should be differentiated from pigment precipitates associated with pigment dispersion syndrome, pseudoexfoliation syndrome, or any other condition that may cause pigment discharge into the anterior chamber. Pigment dispersion syndrome typically causes a perpendicular line of pigment deposition defined as a Krukenberg’s spindle.17 There are also recently described entities of pigment dispersion that may masquerade anterior uveitis.18,19 In both bilateral acute depigmentation of the iris (BADI) and bilateral acute transillumination of the iris (BAIT), the finding of corneal endothelial pigment precipitates is a useful clue to the differential diagnosis.18,19
Anterior Chamber Flare
Aqueous humor is a transparent liquid in healthy eyes. Breakdown of the blood-aqueous barrier causes protein exudation into the anterior chamber. Increased protein concentration of the aqueous humor causes an optical phenomenon called flare or Tyndall effect.20 The grading of flare in the anterior chamber helps to assess the severity of anterior uveitis and has importance in monitoring the patients’ response to therapy. Flare can be clinically graded on a 0 + to 4 + scale at the slit lamp.21 A beam 1 mm wide and 3 mm long is used with the highest light intensity and 16 x magnification at the slit-lamp. The score of 1 + corresponds to faint flare, 2 + corresponds to moderate flare (iris and lens details clear), 3 + to marked flare (iris and lens details hazy) and 4 + to intense flare (fibrin or plastic aqueous). However slit-lamp assessment of flare is subjective and imprecise.
Laser Flare Photometry (LFP) is a quantitative and automated technique that can measure flare. It is the only objective way to measure intraocular inflammation.22 It was shown to be most useful in anterior uveitis.23 Flare measurements by LFP provide precise monitoring of inflammation and can be used to adjust the management of both acute and chronic anterior uveitis. LFP flare has been reported to be a more sensitive parameter than slit-lamp grading of cells in assessing evolution of HLA-B27-associated acute anterior uveitis.24 Several groups have reported that LFP flare was the most important inflammatory parameter in children with Juvenile Idiopathic Arthritis (JIA)-associated chronic anterior uveitis and high flare values were correlated with poor visual acuity and a higher prevalence of ocular complications.25–28
Aqueous Cells
Anterior chamber cells are primarily lymphocytes in most episodes of anterior uveitis, but a significant number of neutrophilis may be present early in the course of disease.8 The intensity of the cellular reaction in the anterior chamber is graded according to the number of inflammatory cells in the 1 x 3 mm slit-lamp beam. The level 0.5 + corresponds to (1–5) cells, 1 + corresponds to (6–15) cells, 2 + corresponds to (16–25) cells, 3 + corresponds to (26–50) cells and 4 + corresponds to more than 50 cells.1
When there is an excedingly high amount of leukocytes in the aqueous, they precipitate with gravity and form an accumulation in the anterior chamber angle that is referred to as a hypopyon formation. Various inflammatory, infective and neoplastic conditions can cause a hypopyon.29 Hypopyon is a nonspecific sign, more often seen in HLAB27 related uveitis and Behçet’s uveitis. Hypopyon in Behçet’s uveitis shifts freely with head positioning, forms a smooth layer, and dissolves rapidly (see Figure 1). By contrast, in HLA B27 related uveitis, hypopyon is always sticky and does not move freely with position.29,30 Other noninflammatory particles in the aqueous humor should be differentiated from inflammatory cells. Erythrocytes, ghost cells, debris, and pigment particles may be seen circulating in the anterior chamber in nonuveitic conditions such as trauma, pigment dispersion syndrome (PDS) and pseudo exfoliation syndrome (PXS);31,32 but also in uveitis patients with ocular complications that may result in dispersion of such particles in the anterior chamber.
Iris and Trabecular Meshwork Nodules
Iris nodules are accumulations of leukocytes on the anterior iris and they represent granulomatous uveitis. Iris nodules are called Koeppe nodules when they are seen at the pupillary magrin and Busacca nodules when they occur on the iris stroma (see Figure 2). Iris nodules are more specific than granulomatous KPs for granulomatous uveitis such as tuberculosis and sarcoidosis. Multiple, small, nonsticky Koeppe nodules and diffuse Busacca nodules are often associated with Fuchs Uveitis Syndrome (FUS). 9 In ocular sarcoidosis, small nodules are commonly seen on the surface of the trabecular meshwork (TM) and are also named as Berlin nodules. Gonioscopic examination with high magnification may help to detect the TM nodules.33 Pupil Changes In acute iritis and iridocyclitis, miosis occurs due to iris edema and sphincter muscle spasm. In contrast, a dilated or distorted pupil with spiraling of the iris 11 may be associated with herpetic uveitis (see Figure 3). Diffuse iris atrophy in FUS may be associated with a slightly larger pupil compared to the fellow eye. 34 Anterior and Posterior Synechiae Adhesions between the anterior lens surface and the iris are named as posterior synechiae and adhesions in iridocorneal angle are named as anterior synechiae. Permanent synechiae are suggestive of previous uveitis attacks. Adherent pigment clumps or a ring of pigment on the surface of the crystalline lens suggests broken synechiae following an episode of severe fibrinous acute anterior uveitis and is commonly seen in eyes with HLA-B27-associated anterior uveitis. (see Figure 4) The finding of broad- based, persistent posterior synechiae is considered one of the diagnostic clues for ocular tuberculosis.35 Extensive posterior synechiae is a common complication of JIA-related chronic iridocyclitis. Posterior synechiae extending for 360 degrees are called seclusio pupilla and lead to pupillary block glaucoma. Anterior synechiae can cause angle closure glaucoma. The tent-shaped anterior synechiae are suggestive of ocular sarcoidosis.33 In general, the presence of synechiae shows that inflammaton is recurrent or chronic. However, these adhesions may also develop within a few days after a severe uveitis attack.
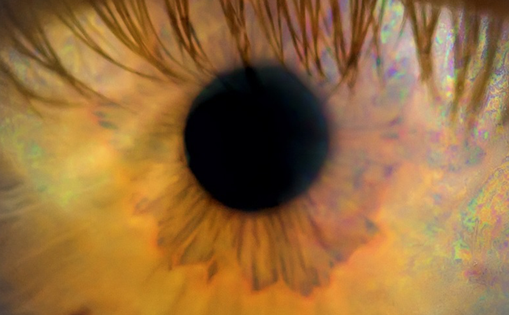
Iris Atrophy
The iris atrophy in Herpes Simplex Virus/Varicella Zoster Virus (HSV/VZV) anterior uveitis is characteristically patchy or sectoral and may be associated with transillumination defects.10 Radial midperipheral transillumination defects occur in PDS. Transillumination defects at the pupillary margin may be seen in PXS.32,36 Both PDS and PXS may sometimes mimic anterior uveitis. A diffuse iris atrophy develops in FUS and causes loss of corrugated texture of the iris stroma.16 In unilateral FUS, heterochromia develops typically with hypochromia of the involved eye. However, in patients with light blue iris color, an inverse heterochromia may be observed. Heterochromia is much less common in FUS patients with dark brown eyes.9
Changes in lens
Inflamatory cells and pigment deposits can cause a fibrinoid membrane on the lens surface. Complicated cataract may be seen as a result of thickened lens capsule, altered membrane permeability, and the use of topical corticosteroids.
Intraocular pressure changes: Intraocular inflammation may lead to raised intraocular pressure (IOP) by several mechanisms. Inflammatory cells in uveitis may block trabecular meshwork. Increased aqueous viscosity may reduce outflow facility and secondary structural changes such as peripheral anterior synechiae (PAS) or posterior synechiae with iris bombe may cause mechanical blockage.37,38 Furthermore corticosteroid treatment is the most common cause of IOP elevation in uveitis.39 Corticosteroids may prompt IOP elevations both by an increase in aqueous secretion and a reduction in outflow.40 In particular, IOP elevations occur with greater frequency in uveitis patients receiving intravitreal triamcinolone enjections.41 Patients with chronic uveitis are more likely to have raised IOP and glaucoma. This complication is more commonly associated with certain uveitic entites such as FUS, sarcoidosis, JIA-associated chronic anterior uveitis, and viral anterior uveitis.42–45 On the other hand, acute anterior uveitis episodes can result in reduction of IOP. Severe inflammation of ciliary body may lead to decreased aqueous production and increased uveoscleral outflow.46 Consequently, transient hypotony can be seen in exacerbations of anterior uveitis such as HLA-B27 related acute anterior uveitis. Persistent hypotony, on the other hand, may result from ciliary body atrophy and/or ciliary detachment caused by a cyclitic membrane formation. Persistent hypotony is considered as the most severe complication of chronic anterior uveitis.
In conclusion, anterior uveitis can have a benign clinical presentation but can cause serious complications if not diagnosed and treated on time. Recognition of ocular diagnostic clues is essential in making a clinical diagnosis of specific entities as well as in guiding diagnostic investigations in patients who present with anterior uveitis.