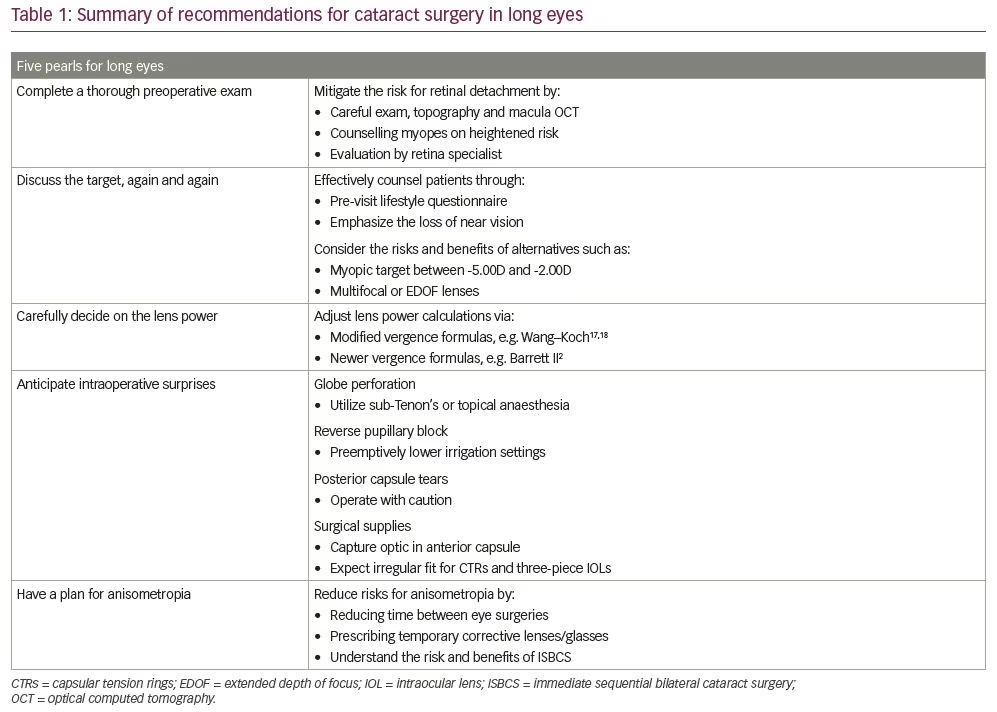
Primary myopia is a refraction anomaly of a non-accommodated eye with a spherical equivalent of -0.5 dioptres (D) or lower, often caused by an elongation of the visual axis.1 While visual axis length often varies between individuals and populations, a ‘long eye’ is often defined by an axial length greater than 24.5 mm.2 The aberrant anatomy of long eyes, which includes longer axial lengths, larger sulcus spaces and larger white-to-white ratio, presents unique challenges for cataract surgery. We provide five pearls for optimizing cataract surgery for patients with long eyes (Table 1).
Pearl 1: Complete a thorough preoperative exam
Rhegmatogenous retinal detachment (RRD), the most common form of retinal detachment, is defined as a tear the retina which allows fluid to flow from the vitreous cavity into the subretinal space, creating retinal separation.3 Cataract surgery is an independent risk factor for RRD, due to the resulting accelerated liquefaction of the vitreous humor.4 Myopia, which is also associated with enhanced vitreous liquification, further compounds the risk of retinal detachment.5–8 Presence of a posterior vitreous detachment prior to cataract surgery can be protective for retinal detachment, although patients still have a higher risk.9 Studies have estimated an increased risk of 2.7–18.9x for pseudophakic myopes versus pseudophakic non-myopes.10 Thus, additional diligence is required when operating on long eyes.
We recommend the following precautions to mitigate the risk of RRD. First, a thorough preoperative examination of the lens and the retina should be performed. Specifically, peripheral examination and imaging, including topography and macular optical coherence tomography, should be completed when appropriate. Second, patients should be counselled and educated on the added operative risks associated with myopia. Finally, in patients at high risk for retina complications, a supplementary evaluation by a retina specialist should be considered, not only to rule out asymptomatic retinal tears or holes, but also to proactively connect the patient with a retina clinic that the patient can call for any future myopia-related retinal complications.
Pearl 2: Discuss the target, again and again
Patients with long eyes often require comprehensive counselling and education regarding the loss of near vision when given distance vision in both eyes. This trade-off may need to be reiterated with the patient several times to ensure understanding. Though these conversations may feel frustrating or circular, the surgeon is an invaluable guide for these patients and intentional,
preoperative discussion is a necessity.
We suggest the following actions to enhance patient counselling. Firstly, consider asking patients to complete a pre-visit lifestyle questionnaire regarding their interests and priorities. This survey may prepare surgeons for patient expectations and streamline counselling conversations. Secondly, a patient should be counselled about loss of near vision with a monofocal lens aimed for distance. Key questions include: “do you take off your glasses to read at night?” Or: “do you take off your glasses to check your cell phone?” Emphasizing the loss of near vision is important for these activities. If the patient has a clear understanding, or a history of wearing contact lenses for distance with readers on top, bilateral emmetropia may be considered. If the patient is not accepting of loss of near vision, the surgeon can instead offer the option of keeping the patient myopic between -5.00 D to -2.00 D with prescribed reading glasses, if such a situation better aligns with the patient’s preference. Monovision is a third option that can be offered, but is best tried prior to surgery or with a successful history of monovision in contact lenses.
Multifocal or extended depth of focus (EDOF) lenses can also be utilized. However, special consideration is required when evaluating premium lenses. In mild to moderate myopes, near-vision quality may be worse in multifocal lenses or EDOF lenses compared to pre-surgical near-vision quality with glasses removed. For patients who never remove their glasses to read, this trade-off is less concerning. These patients are usually higher myopes and could be good candidates. In addition, multifocal lenses may affect postoperative visual quality due to an amplified angle kappa.11 Finally, lens choice may complicate future retinal surgery, both from an imaging12 and an intraoperative visibility standpoint.13 Overall, these presbyopia-correcting lenses can be excellent for patients, but careful preoperative exam and counselling is important.
Pearl 3: Carefully decide on the lens power
Traditional vergence formulas assume a single global index of refraction for lens power calculations. However, eyes with a longer axial length will have a larger vitreous cavity; Thus, these formulas have the potential to underestimate lens power, leading to hyperopic surprise. In addition, techniques such as partial coherence interferometry, while more accurate than conventional ultrasound, assume the anterior chamber and axial length are proportional, which may also disrupt lens power calculations.14–16
We advise that surgeons adjust their lens power calculations, either by modifying traditional vergence formulas or employing newer formulas that account for varying axial length. Axial length modifications, such as the Wang–Koch adjustment to Holladay 1, have been proven to reduce hyperopic outcomes in myopic patients.17,18 These modified traditional formulas appear to be as accurate for myopes as newer-generation formulas,19 and may even be more accurate.20
Alternatively, newer-generation formulas, which may better account for axial length variation, may also be utilized for myopes. Prior studies have reached differing conclusions regarding the best formula for long eyes. Previous analyses have suggested the SRK/T,21 Barrett Universal II,22–26 Haigis,27–29 Hill-RBF 2,30,31 or Olsen formulas are preferred. Some studies have shown head-to-head myopic performance between formulas can vary based on the specific characteristics of a given subgroup,32,33 and other studies have shown no significant myopic performance differences between formulas.34,35 However, a 2018 meta-analysis of 11 observational studies demonstrated the superiority of Barrett Universal II over Holladay 2, SRK/T, Hoffer Q and Holladay 1 in predicting intraocular lens (IOL) power in long eyes.2 Newer formulas, such as Barrett and Kane, can offer improved outcomes in long eyes.22 In particular, the Kane formula has been shown to be superior to all the formulas described.36 In addition, intraoperative aberrometry can offer additional data to improve outcomes, although studies show modern formulas are similar in outcomes.37–40
Our clinic’s best practices include utilizing a Barrett II and adjusted Holladay I. Surgeons may also consider operating on the non-dominant eye first with a slight myopic aim, then factoring in refractive predictive error from the first eye into their lens power calculations for the second eye.
Pearl 4: Anticipate intraoperative surprises
The risk of intraoperative complications may be enhanced in long eyes. For example, the risk of globe perforation from peribulbar and retrobulbar nerve blocks is elevated in eyes with greater axial length.41,42 When local anaesthesia is indicated, we advocate for topical anaesthesia or a sub-Tenon’s block, rather than a peribulbar or retrobulbar block.43
Reverse pupillary block is caused by increased anterior chamber pressure compared to posterior chamber pressure, which seals the iris posteriorly against the anterior lens capsule, creating a deeper anterior chamber. While reverse pupillary block can be caused by excessive pressure from irrigation during any cataract surgery, longer eyes may carry a higher risk due to their larger anterior chamber volume, which affects phacodynamics. In addition, posterior chamber volume is also increased, creating greater aqueous humour flow into the anterior chamber.44,45 When encountering reverse pupillary block, surgeons should carefully raise the iris with a blunt instrument to restore flow. Surgeons may also consider pre-emptively lowering their irrigation settings during the operation. The risk of tears in the posterior capsule of the lens is also increased in long eyes.46,47 In addition, high myopia can be a risk factor for zonular weakness.48 Thus, surgeons should complete phacoemulsification and irrigation/aspiration in myopes with particular caution, regardless of their experience level or tenure.
Finally, the anatomical irregularities of a long eye may impact surgical supplies. For example, anterior chamber lenses are sized based on the white-to-white corneal diameter, which is the horizontal distance between the borders of the corneal limbus, and capsule tension rings are based on estimated bag size, which is derived from estimated axial length. Because the white-to-white is increased in long eyes,49 capsule tension rings are not ‘one size fits all’, and the fit may be different than expected. Similarly, a larger white-to-white may allow dislocation of three-piece IOLs due to the IOL diameter lacking enough width to fill the haptic-to-haptic in larger eyes. We recommend capturing the optic in the anterior capsule to avoid movement in the sulcus space in the event that the IOL is not be safely implanted into the bag. Surgeons should be aware of these risks and plan their surgical supplies accordingly.
Pearl 5: Have a plan for anisometropia
In the time between surgery on a patient’s first and second eye, anisometropia can be not only disconcerting, but also potentially dangerous for patients, due to an increased risk of falls.50 We propose the following solutions to help anticipate and curb the effects of anisometropia: First, surgeons should consider reducing the time between eye surgeries to reduce the period of anisometropia. Second, surgeons should consider placing a contact lens or prescribing temporary glasses until the second surgery is completed.
Immediate sequential bilateral cataract surgery (ISBCS) is commonly performed outside the United States, and its safety, efficacy and efficiency have been extensively studied.51,52 One benefit of ISBCS is the lack of an anisometropia period for patients. However, ISBCS, just like every other surgical technique, encompasses a unique portfolio of risks and benefits, which is outside the scope of this review. Nevertheless, surgeons should be cognizant of the range of options for addressing the temporary anisometropia between eyes.
Conclusion
In conclusion, long eyes present unique challenges for cataract surgeons. We provide five pearls for guidance surgeons to optimized surgical outcomes and patient satisfaction.