As the percentage of elderly people that make up the population of the USA grows, it is imperative to shift our focus on how to best address their needs and outline an approach to the geriatric eye. This review describes common physiologic and pathologic conditions affecting the aging eye including presbyopia, posterior cortical atrophy, giant cell arteritis (GCA), sagging eye syndrome, strokes, progressive supranuclear palsy (PSP), and non-arteritic anterior ischemic optic neuropathy (NAION).
Presbyopia
Accommodation is the ability of the native lens and zonules to increase their refractive power to keep objects that are closer to the eye in focus on the retina, and vice versa.1 Presbyopia is the gradual age-related loss of the ability to accommodate, and the most significant loss of this ability occurs after approximately 50 years of age. Under the age of 20, the normal accommodative power of the eye is 7–10 diopters, but by age 50, it decreases to about 0.5 diopters.2 Symptoms of presbyopia are usually first reported around 42–44 years of age, and there is considerable reduction in amplitude of accommodation by age 50–55 years. Patients typically present with blurred vision at near and asthenopia (e.g., squinting, headaches secondary to eye strain), increased light requirement, and the need to work from progressively greater distances.1,3 To diagnose accommodative insufficiency, a clinical exam measuring corrected near and distance visual acuities needs to be carried out to measure refractive error and functional capacity at near distances. Cycloplegic retinoscopy and refraction might uncover latent hyperopic refractive error that might contribute to symptoms of accommodative insufficiency, including presbyopia.
While presbyopia is inherent to the process of aging, the exact pathophysiology of it is still ill defined.1 While the exact cause is unknown, there have been two categories of thoughts that have developed as possible explanations for the development of presbyopia: lenticular and extralenticular.4 The lenticular theories suggest that presbyopia results from structural changes (e.g., sclerosis of the nuclear lens tissue, decreased distance between ciliary muscle and the lens equator, decreased elasticity of the lens capsule) that occur in the lens, capsule or zonular fibers. Extralenticular theories suggest that presbyopia may result from ciliary muscle dysfunction, loss of elasticity in the posterior zonules or choroid, and/or decreasing resistance of the vitreous humor against the accommodating lens capsule.4–6 Although age is the primary factor determining the development of presbyopia, other factors that may cause premature onset of presbyopia include systemic disease, medications, and trauma.7,8
Presbyopia is preferably managed with corrective glasses (e.g., bifocals, progressive lenses) for near work; however, surgical options may also be helpful (e.g., intraocular multifocal lenses, and corneal inlays).8 These interventions may increase the depth of the field, but at the possible cost of loss of contrast or best-corrected visual acuity.9,10
Posterior cortical atrophy—visual variant of Alzheimer’s disease or Benson’s syndrome
Posterior cortical atrophy (PCA) is a neurodegenerative syndrome in which patients develop progressive higher order visual function loss, but could have relatively unaffected cognition. PCA presents in patients in their
mid-50s or older, and there are generally no initial abnormalities noted on routine ophthalmic and neurologic exam. Some studies have reported a slight female bias,11,12 but others have found no gender preference.13,14 Symptoms usually have visuospatial manifestations, such as difficulty with reading, navigating, numeracy, and interpretation of complex scenery despite normal visual acuity and normal structural eye exam, or disproportionate to their underlying ocular morbidity including cataract, age-related macular degeneration etc. Over time, a homonymous hemianopsia or cortical visual loss may develop. Tests that may help indicate PCA that can be conducted in the clinic include the clock-drawing test for visuospatial deficits, and the cookie theft test (simultagnosia). Making use of Ishihara color plates may also help narrow down the diagnosis, as patients with PCA may be unable to verbalize the embedded number, despite the ability to identify the colors or even the ability to trace the number with their finger (simultagnosia).
Diagnosis may be made with radiographic findings (e.g., magnetic resonance imaging [MRI], positron emission tomography) suggestive of posterior (parieto-occipital) brain atrophy. There may be relative sparing of the medial temporal lobe.12,15 The pathological basis for this condition is analogous to that of Alzheimer’s disease as patients with PCA are noted to have neurofibrillary tangles and amyloid plaques on autopsy.11,14 PCA and Alzheimer’s disease may also result in cerebrospinal fluid containing phosphorylated tau and beta amyloid.16–19 The genetics of the condition are being studied and a large genome-wide association study of 302 patients with PCA has identified three loci (SEMA3C, CNTNAP5, and FAM46A) of interest.20
There have been two proposed subtypes of PCA: the occipito-parietal and the ventral, based on which cortical visual stream is affected by the neurodegeneration.21–24 When the occipito-parietal stream is affected, then it results in visuospatial complaints, and when the ventral stream is affected it results in visuo-perceptive difficulties (e.g., visual agnosia, simultagnosia, prosopagnosia, and agraphia). However, some researchers argue that PCA is a continuum, rather than consisting of two distinct subtypes.12,25 Patients with PCA typically progress to develop episodic memory loss, and linguistic and executive dysfunction.11,12,26
Management is mostly supportive but there is a heavy focus on improving the quality of life and maintaining the activities of daily living in these patients via occupational therapy and visual rehabilitation. Acetylcholinesterase inhibitors (e.g., donepezil, galantamine, rivastigmine) are used for treatment of Alzheimer’s disease and there have been some case reports suggesting that they may be useful in the treatment of PCA.25,27
Giant cell arteritis—temporal arteritis
GCA is the most common vasculitis in patients over the age of 50 and has a higher prevalence in Caucasians, specifically those of Scandinavian and Northern European descent.28–31 The average age of presentation is
72.5 years in women and 70.3 years in men, and it is twice as common in women.29,31,32 GCA is a granulomatous inflammation of medium- to large-sized vessels. The most common vessels that are implicated in this condition are the branches of external carotid, internal carotid, and the vertebral arteries.33 Involvement of the ophthalmic artery as well as the posterior ciliary arteries are responsible for the severe visual morbidity in affected patients. GCA typically presents to ophthalmology with acute unilateral or bilateral vision loss34,35 and associated symptoms of headache (temporal or occipital),36,37 scalp tenderness, jaw claudication, diplopia, myalgias, and constitutional symptoms.38 GCA is considered an ophthalmologic emergency because if left untreated it may progress to permanent vision loss (usually secondary to arteritic anterior ischemic optic neuropathy, but also to posterior ischemic optic neuropathy, or central retinal artery occlusion).34 Although the gold standard for diagnosing GCA is the temporal artery biopsy, the results of these biopsies may be falsely negative due to GCA containing skip lesions. Erythrocyte sedimentation rate and C-reactive peptide lab tests can support the diagnosis of GCA.36,39–41
The exact cause of GCA is still unknown; some studies conducted in a stable population appeared to show cyclic fluctuation in the incidence of GCA, supporting an infectious (Chlamydia pneumoniae, varicella, parvovirus B19), environmental, or genetic cause of GCA,36,42–44 while others suggest that GCA is an endogenous inflammatory event caused by an element in the arterial wall.45 In response to the unknown initiating event, T cells in the vessels upregulate macrophages, causing a granulomatous immune reaction. This reaction results in the destruction and remodeling of the arterial wall and progresses to occluding the lumen, resulting in the ischemic symptoms of GCA.46
Corticosteroids are the mainstay of treatment upon initial diagnosis.47 In GCA, interleukin-6 (IL-6) is one of many inflammatory mediators that is predominantly upregulated in the inflamed arteries. There has been a recent trial investigating the benefits of tocilizumab (an anti-IL-6) in patients with refractory GCA or those with significant steroid-related side effects. Tocilizumab helps to taper steroid treatment faster while keeping the inflammation in GCA under control.48,49 While the effectiveness of treatment is highly dependent on how quickly it was initiated, up to one third of the treated cases may show some level of improvement in visual acuity, however, prognosis in affected eyes is usually poor.50–53
Sagging eye syndrome
Sagging eye syndrome is an increasingly recognized cause of strabismus in the elderly population. The extraocular muscles are surrounded by connective tissue that functionally serves to support and act as pulleys for the extraocular muscles. Age-related degeneration of this connective tissue results in “sagging” and can cause esotropia, hypotropia, supraduction deficit and/or strabismus. An orbital MRI may show the lateral rectus–superior rectus connective tissue sagging.54 Patients who are not experiencing double vision are typically managed expectantly. Otherwise, patients are offered prisms to manage the double vision. There are also surgical options for treatment of sagging eye syndrome if they do not respond to, or do not want, prism therapy.
Strokes
The eyes and brain share a vascular supply, so transient vision loss can be a warning sign for an imminent stroke and should be treated as thus.55 Amaurosis fugax is commonly caused by carotid insufficiency and nearly 50% of these cases progress to cause a stroke within 3 years. Hypertension, diabetes, hypercholesterolemia, and cardiovascular risk factors increase overall risk for stroke. New-onset neurologic deficits, such as monocular vision loss from arterial occlusion, binocular acute onset homonymous field defect, acute onset binocular horizontal or vertical diplopia including transient vision loss, are red flags for stroke and need to be evaluated by stroke neurology for detailed imaging and stroke work-up, as well as management of systemic risk factors.
Progressive supranuclear palsy—Steele–Richardson–Olszewski syndrome
PSP is a tauopathy that typically presents in adults older than 40 years of age,56,57 but can easily be misdiagnosed as other neurodegenerative conditions like Parkinson’s disease.58 Patients with PSP usually present with progressive supranuclear vertical ophthalmoplegia, that is more apparent in the downgaze, and postural instability.59–61 These symptoms can be attributed to the degeneration of neurons secondary to accumulation of tau proteins in the brainstem and basal ganglia, superior to the nuclei that control eye movement.62,63 An MRI may be performed to rule out other causes for the symptoms such as cerebrovascular disease, hydrocephalus, and tumors. An MRI for PSP may reveal atrophy of the midbrain, poor differentiation of the substantia nigra and atrophy of the putamen and/or red nucleus, commonly referred to as the “hummingbird sign”.64 The exact cause of PSP is unknown but it has been attributed to arsenic, and genetic mutations that result in neurofibrillary tangles.65–68
While there are no effective medications to treat PSP, symptomatic treatment and physical therapy for fall reduction should be offered to patients. Dopaminergic replacement therapy may mildly relieve symptoms temporarily. Antidepressants are helpful in treating associated symptoms of apathy or depression. Amitriptyline may be used to alleviate the insomnia and gabapentin may be used to treat dystonic pain. Mirror-prism glasses may help the downgaze palsy and botulinum toxin injections may reduce blepharospasm, dystonia, and retrocollis.69,70 The prognosis for PSP is poor, with average time of survival from diagnosis being 5–9 years.70,71
Non-arteritic ischemic optic neuropathy
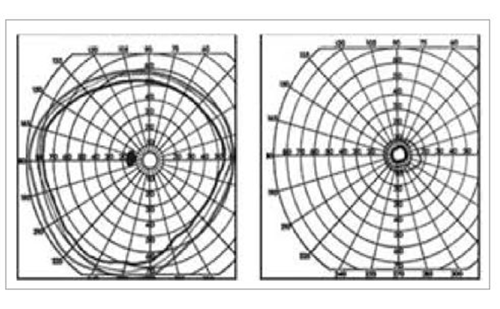
NAION is the most common acute optic neuropathy in patients over 50 years old.72–74 Patients typically present with acute, unilateral painless vision loss or blurring, typically sectorally in the inferior visual field. Patients have decreased visual acuity, visual field defects, relative afferent pupillary defect, and a swollen optic nerve on physical exam.75–77 NAION is typically associated with vasculopathic risk factors, but other factors have also been proposed (e.g., sleep apnea syndrome,78,79 interferon alpha medication,80,81 phosphodiesterase inhibitors,82 and optic disc drusen).83–85 The pathophysiological mechanism has been suggested to be that NAION is a result of insufficient circulation in the short posterior ciliary arteries.86–89
There is no clinically proven treatment for NAION. The role for anticoagulants and antiplatelet agents, and use of steroids in the therapy of NAION, however, is without proven benefits.90,91 Control of systemic risk factors including diabetes, hypertension, and hyperlipidemia with regular exercise, aspirin (unless contraindicated), and dietary modification may be advised to the patient to reduce the risk of involvement of the other eye. The vision changes associated with NAION typically stabilize within 2 months of onset.76 Currently there are ongoing clinical trials for therapeutic intervention in NAION, both in the acute and chronic setting, and the options of enrollment in a trial may be discussed with the patient.92 The prognosis for visual recovery is better in younger patients.74
Summary
The ocular conditions that present in the elderly are very distinct compared with the pathologies presenting in the younger population. Most general practitioners are aware of some common problems, such as cataract and glaucoma, and refer them to ophthalmologists. However, there are some less well-known neuro-ophthalmic conditions which, if not identified in a timely manner, can lead to irreversible vision loss and compromise quality of life for the elderly, many of whom are already dealing with multiple comorbidities. Several recent studies have also linked vision loss with depression and earlier onset of neuro-cognitive disorders. Identification and timely referrals can sometimes salvage vision, especially when time is a crucial factor, as in GCA. Some conditions, such as NAION, are associated with multiple systemic risk factors that need to be adequately controlled to the reduce risk of involvement of the other eye. These conditions require a multidisciplinary approach, requiring input from primary care physicians, ophthalmologists and also neurologists.