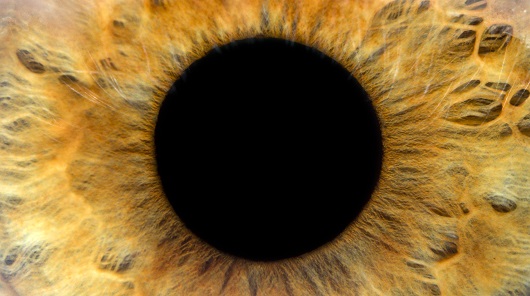
Keratoconus is the most common primary progressive ectatic condition of the cornea. It is classically described as non-inflammatory, distinguishing it from several other pathologies associated with corneal thinning. Prevalence of this disease varies depending on geographical location, with reports as high as 2.3% in Central India to 0.3% in Russia.1,2 Keratoconus typically presents as a bilateral condition although approximately 14% of patients may demonstrate unilateral disease.3 Keratoconus occurs in both males and females, typically around the second decade of life. The aetiology behind the progressive corneal thinning and steepening is not completely understood; however, independent risk factors include a positive family history, eye rubbing, asthma, allergy and eczema.4 Ocular findings and self-reported symptoms depend on severity of progression. Early in the disease course, patients present with significant refractive error due to asymmetric astigmatism and progressive myopic shift. Left untreated, individuals may develop breaks in Bowman’s membrane, tears in Descemet’s membrane and ultimately severe stromal scarring.5 As our understanding and detection of keratoconus advances, so do the treatment and management options for this disease. This article aims to outline both traditional and novel therapeutic options for keratoconus.
PubMed and MEDLINE were searched for peer-reviewed literature on treatment of keratoconus. Search criteria included keywords of ‘keratoconus treatment’, ‘corneal crosslinking’ and ‘intracorneal ring segments’. The following discussion describes the current treatments available, including some therapies that are not currently approved by the US Food and Drug Administration (FDA) and are strictly off label for the treatment of keratoconus.
Rigid gas permeable and scleral contact lenses
One of the least invasive options for patients with progressive keratoconus is the fitting of rigid gas permeable and scleral contact lenses. Rigid gas permeable (RGP) contact lenses allow the cornea to adopt a spherical shape due to tear collection behind the lens. The combination of the rigid lens and tear collection behind the lens functions to neutralize existing irregularity from the ectasia while correcting for the patient’s underlying refractive error. The primary complaint associated with RGP lenses is discomfort, at which point practitioners can offer scleral lens fitting.6 Scleral lenses contain a rigid centre, with a softer periphery leading to improved patient tolerability. A 2020 randomized controlled trial reported significantly better comfort ratings for patients wearing scleral lenses compared with RGP lenses.7 There does not appear to be any significant difference in visual acuity between the two options.7 Additionally, a 2016 retrospective case series in Canada determined the scleral lens to be an acceptable alternative for those who cannot tolerate RGP lenses.8
Epithelium off corneal crosslinking
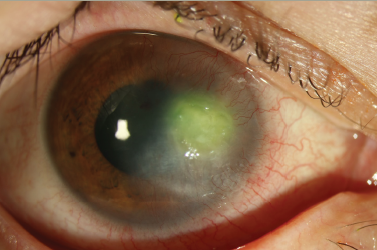
Corneal collagen crosslinking (CXL) is currently the treatment of choice for progressive keratoconus. The goal of CXL is to strengthen corneal stromal fibres in an effort to stabilize the ectatic disease and mitigate further progression. The procedure combines topical riboflavin (vitamin B2) drops and ultraviolet light (UV-A) to strengthen collagen fibres in the cornea. Upon exposure to UV-A light, a photochemical reaction causes the release of reactive oxygen species, resulting in the formation of covalent bonds between collagen and proteoglycan fibres.9 This reaction is similar to the molecular changes that occur with the natural ageing process of the cornea. It should be noted that CXL is not recommended in a stable disease state, but rather in cases of progressive disease or when there is ectasia present after refractive surgery. The most common iteration of the procedure is epithelium-off (epi-off) CXL, during which the corneal epithelium is mechanically removed before topical 0.1% riboflavin is applied to the surface at intervals of 2–5 minutes for 30 minutes. Following application of the riboflavin, the surface is irradiated with UV-A, inducing the photochemical reaction as previously described. Patients are typically given topical antibiotics and steroids after the procedure, followed by a brief regimen of steroids after re-epithelialization occurs. This technique is called the Dresden protocol, established by Dr Seiler et al. after introducing the concept of CXL in 2003.10 Some pitfalls to epi-off CXL include slowed corneal re-epithelialization, which leads to heightened infection risk. In addition, patients often report significant discomfort after the procedure, which can limit its utility in children. A soft bandage contact lens is often applied after the procedure to promote healing of the epithelium. Newer studies demonstrate a matrix therapy agent (ReGeneraTing Agent, RGTA) to promote faster corneal healing and thus a decreased risk of infection, with additional relief in postoperative discomfort.11 Finally, damage to the corneal endothelium upon exposure to UV-A light has been reported, particularly in patients with corneal thickness below 400 microns at the time of exposure to UV-A application. Given the progressive corneal thinning that occurs with keratoconus, a large portion of the population fall into the aforementioned category and are not acceptable candidates for CXL.12
Epithelium on corneal crosslinking
Due to unfavourable side effects of epi-off CXL, there has been newer interest in epithelium-on (epi-on) or transepithelial CXL. The procedure follows similar principles to epi-off CXL; however, as indicated in the name, the corneal epithelium remains intact. The challenge with epi-on CXL is ensuring that topical riboflavin penetrates to the stromal layers. This issue has been addressed by a variety of methods, including alteration of the concentration of riboflavin, partial micro-puncture of the epithelium, and iontophoresis, which utilizes an electrical gradient to drive riboflavin molecules across the corneal endothelium.13 A 2016 systematic review reported that patients receiving epi-on CXL demonstrated a statistically significant improvement in uncorrected distance visual acuity (UDVA), while there was no significant change in Kmax at 3–12 months’ follow-up. An additional systematic review comparing epi-off versus epi-on CXL found no significant difference in UDVA and corrected distance visual acuity (CDVA) at 1-year follow-up between the groups.14 A primary limitation in evaluating outcomes in epi-on CXL is that there is no single protocol currently utilized by each provider, leading to poor repeatability. Additionally, epi-on CXL has not at this time been cleared for FDA approval in the USA; therefore, its use is strictly off label.
Accelerated crosslinking
Many investigators have pursued alterations to the Dresden protocol to further optimize surgical management of keratoconus. One such technique is accelerated CXL, which aims to maintain the same efficacy as traditional CXL, with the benefits of a shorter procedure.15 Similarly to epi-on CXL, several iterations of accelerated crosslinking exist. The accelerated timeline involves increasing UV-A illumination during the procedure, thereby decreasing UV-A exposure time. A prospective interventional case series investigated high-fluence pulsed UV-A at 30 mW/cm2 for 4 minutes and studied Kmax values at 24 months as the primary outcome. Accelerated pulsed CXL was shown to be safe and effective, with refractively neutral intervention for mitigating disease progression.16 As previously mentioned, several methods for delivery and illumination levels have been studied, without universal acceptance of a single approach. One current protocol that is being studied extensively is the use of supplemental oxygen therapy during accelerated crosslinking.17 In one of the pathways of corneal crosslinking, singlet oxygen species are generated when excited riboflavin reacts with oxygen. In accelerated crosslinking, there is evidence to support that an alternate low-oxygen reaction pathway is activated more quickly, resulting in decreased efficacy of crosslinking treatment.18 Ongoing debate exists on whether accelerated crosslinking protocols, with or without oxygen supplementation, offer comparable or superior efficacy when compared with conventional crosslinking therapy.
Customized crosslinking
Newer techniques using topography-guided customized corneal crosslinking (PiXL) have provided a more targeted area of treatment to the focal areas of biomechanical weakening in the ectatic cornea. PiXL has shown efficacy in reducing higher-order aberrations, improving best spectacle-corrected distance visual acuity (BSCVA) and hastening epithelial healing compared with standard, generalized crosslinking treatment.19 In PiXL, there is debate on whether to apply treatment to the highest keratometry value, thinnest pachymetry point or posterior float. Seiler et al. described the posterior float as the most reliable parameter for targeted treatment, arguing that pachymetry and highest keratometry are both modulated by epithelial thickness.20 PiXL has shown promising results for patients with keratoconus, as well as in patients with myopic or astigmatic refractive error. Larger sample sizes and long-term data collection are needed to determine the efficacy of this procedure compared with standard CXL.
Intracorneal ring segments
The principle of intracorneal ring segments (ICRS) was initially adopted for treatment of severe degrees of myopia. Placement of the segments involves insertion of synthetic semicircular inserts into the mid-peripheral corneal stroma. Pressure exerted by the intrastromal rings creates a shortening of the central arc length, resulting in central corneal flattening as well as forward displacement of the peripheral cornea.21 The desired outcome is a decrease in irregular astigmatism, which can improve visual acuity and allow for better refractive correction. A prospective case series evaluating intracorneal ring technology demonstrated a reduction in both astigmatism and spherical correction, as well as an increase in topographical regularity in keratoconus patients.22 Additionally, placement of ICRS resulted in improvement of BSCVA in approximately 50% of patients.23 Common complications associated with placement of the synthetic rings include segment migration, externalization of segment, localized inflammatory reaction, patient intolerance and, in rare cases, overlying stromal melt. Overall, the procedure is well tolerated and can be an effective tool in addressing severe corneal steepening with irregular astigmatism.
Combined intracorneal ring segments and corneal crosslinking
Corneal CXL and ICRS can be used in combination to address severe ectatic disease. When used in combination, CXL works to mitigate the progression of the ectatic cornea and provides biomechanical stability, while ICRS placement works to flatten the cornea and promote topographic regularity. A prospective study suggested that CXL with simultaneous ICRS implantation gives an additional improvement in UDVA with significant reduction in cylinder and spherical equivalent.24 Debate still exists as to which procedure should be performed first, with an additional option of performing the procedures simultaneously. A 2018 meta-analysis reviewing best corrected visual acuity (BCVA) and uncorrected visual acuity (UCVA) outcomes for those patients undergoing subsequent (CXL then ICRS) versus simultaneous procedures found superior refractive outcomes in the patient group undergoing simultaneous procedure.25 Hersh et al. studied the safety concerns and outcomes of simultaneous ICRS and CXL versus ICRS followed by CXL 3 months later.26 Their research showed comparable topographic flattening of the central cone with concurrent ICRS and CXL versus sequential ICRS with CXL. In addition, the side effect profile of combined CXL and ICRS implantation was comparable to that of the respective stand-alone procedures.
Bowman layer inlay transplantation
An additional surgical procedure for progressive keratoconus is transplantation of an isolated Bowman layer graft. Patient selection for this procedure would include patients with advanced progressive keratoconus who are no longer eligible for CXL but still have adequate BCVA.27 The Bowman layer corneal inlay can be inserted via a mechanical tunnel or with femtosecond laser application. Van der Star et al. studied the long-term outcomes of 35 eyes that had undergone Bowman layer inlay transplantation and found stabilization of the corneal curvature in 31 eyes and stabilization of best corrected vision at the 8-year postoperative time point.28 In patients with inadequate stromal thickness, there can be difficulty forming a safe tunnel for the Bowman layer transplant. Bowman layer inlay transplantation can offer an alternative surgical approach to deep anterior lamellar keratoplasty (DALK) and photorefractive keratectomy (PRK) in patients with advanced keratoconus.
Autologous stem cell transplantation
One of the more novel therapies for keratoconus involves implantation of autologous adipose-derived adult stem cells (ADASC) into the corneal stroma. The goal of ADASC implantation is to re-engineer existing tissue of the cornea and to provide an alternative to corneal graft procedures. By inserting stem cells into the scaffolding of the corneal stroma, the cells differentiate into keratocytes and produce new collagen, providing a solution to the underlying pathophysiology of keratoconus.29 A phase I clinical study evaluating the safety and efficacy of ADASC implantation showed no complications and full corneal transparency after 24 hours in all five patients.30 All patients included in the study demonstrated improved visual outcomes, while manifest refraction and topographic keratometry remained stable. This technique offers a promising therapy; however, larger investigative clinical studies need to be conducted before implementation into clinical practice.30
Photorefractive keratectomy
PRK can often be performed in conjunction with CXL to assist in correcting residual refractive error in progressive keratoconus. A 2018 case series showed significant gains in CDVA with no compromise in CXL efficacy over a 24-month follow-up in patients who underwent PRK-CXL.31 Additionally, a prospective study demonstrated an improvement in mean UCVA and BCVA with better vision quality after simultaneous topography-guided PRK followed by CXL.32
Many patients with keratoconus are ineligible to undergo PRK due to severe stromal thinning over the corneal cone. In these cases, transepithelial phototherapeutic keratectomy (t-PTK) can be performed, a procedure that requires less stromal tissue ablation. The combination of CXL and t-PTK is known as the Cretan protocol. A 2019 comparative interventional case series compared the previously mentioned Dresden protocol with the Cretan protocol during CXL, and found significant and faster improvements in refractive and keratometric values in the Cretan group.33 Further investigation has been performed into refractive surgical techniques for those with mild or forme fruste keratoconus. A 2007 prospective study evaluated outcomes of photoastigmatic refractive keratectomy in patients with average keratometry values less than 50.00 diopters.34 The results demonstrated that photoastigmatic correction using the Alpins vector planning technique offered safe and effective myopia and astigmatism correction without sacrificing corneal stability.
Corneal transplantation
For patients with severe disease that is refractory to previous procedural therapies, often the only remaining option is corneal transplantation. Two of the most popular options for corneal transplantation include full-thickness penetrating keratoplasty (PK) and partial-thickness DALK. DALK involves transplantation of the corneal stroma while leaving intact the host Descemet’s membrane and corneal endothelium. A 2019 meta-analysis comparing the two techniques found no difference in BCVA or corneal topography; however, the PK group had a higher rate of transplant rejection and larger residual postoperative spherical equivalent.35 Although DALK is associated with a lower rejection and re-transplantation rate, any concurrent endothelial pathology, such as full-thickness corneal scarring, may preclude DALK as a surgical option. Both primary PK and DALK are useful procedures in the treatment of end-stage keratoconus.
Conclusion
Keratoconus is a commonly encountered disease among ophthalmologists, with numerous therapeutic options available for patients. Regardless of ophthalmic practice, understanding treatment options can benefit patients. Current therapies as discussed above include contact lenses, CXL, ICRS, laser ablation, stem cell transplantation and corneal graft transplantation. Currently, no single perfect management plan exists; rather, each therapeutic plan must be tailored to the patient and to the comfort of the provider. As advances in anterior segment techniques progress, so do the treatment options for keratoconus. The current therapeutic options reviewed in this article aim to improve treatments for patients suffering from this vision-threatening corneal disease.