Visual impairment has a large effect on societal health costs. It has been estimated that the annual cost of major adult visual disorders, including visual impairment, blindness, age-related macular degeneration (AMD), cataracts, diabetic retinopathy (DR), glaucoma and refractive errors, account for a total annual financial burden of $35.4 billion1,2 in the US alone. These costs include direct medical costs, other direct costs and the costs of productivity loss. In Europe, the major causes of serious visual loss are AMD, cataract, DR, glaucoma, and uncorrected refractive errors.3 In 2010, the World Health Organization (WHO) estimated 30 million people in Europe suffered from visual impairment.4 Ageing demographics combined with age-related vision loss is predicted to have a large impact on health and social care service on a global scale. To efficiently treat ocular disorders, surgical procedures must be precise, safe and cost effective. Additionally, precisely targeting the pathological site and defining the required dosage of medication have to be considered. Recently, research has focused more on efficient drug delivery to the eye as well as robotic assistance for surgical procedures in ophthalmology.
This review provides an overview of robotic-assisted ophthalmic surgery as well as recent advances in drug delivery to the posterior eye. Furthermore, we introduce the advantages of magnetic manipulation for minimally invasive ophthalmic microrobots. We demonstrate several magnetically steered tethered and untethered devices as assistive tools for the treatment of specific ocular diseases, such as cataract, AMD, retinal vein occlusion (RVO) and DR.
Robotic Systems for Ophthalmic Surgery
Efficient ophthalmic surgeries must be precise, safe and fast and, thus, require the surgeon to be highly dexterous and experienced as the small forces applied to the structures in the eye are lower than the human force perception limit.5,6 To overcome these limitations, various robotic platforms have been proposed as assistive tools for ophthalmic surgery. Teleoperated systems, such as the da Vinci surgical system7,8 (Intuitive Surgical, Sunnyvale, CA, US), or a parallel robot for vitreo-retinal surgery,9 as well as cooperatively controlled hand-over-hand systems10 and freehand active tremor-filtering systems11 have been suggested to aid in eye surgery. The da Vinci system has been used to close a full thickness corneal and scleral laceration on a porcine eye, but for intraocular surgery the system was unable to create a self-sealing wound in the sclera.8 Parallel robot systems have been proposed for intravitreal surgery, such as retinal vessel cannulation (RVC) or pars plana vitrectomy8 because they can be designed to have a stable remote centre of motion. The steadyhand eye robot was developed at John Hopkins University to actively support the surgeon during an intervention, such as RVC and epiretinal membrane peeling, by cooperatively holding the surgical instrument.10 The Micron is a hand-held system that actively cancels the surgeon’s hand tremor based on low-pass filtering and motion scaling.11 In all these systems the ophthalmic surgeon is still responsible for decision-making and instrument guiding.
Drug Administration to the Eye
The corneal and conjunctival epithelium forms a thick physical barrier that protects the eye from external threats and maintains homeostasis. This barrier must be penetrated if drugs are administered topically to the eye. Studies have shown that eye drops are rapidly lost from the ocular surface due to lachrymation and tear turnover12 and typically less than 5 % of topically applied drugs permeate the eye.13,14
Drug delivery to the posterior segment of the eye, including the retina, vitreous and choroid, requires high doses of medication. Medication is, therefore, commonly delivered intravenously or by intravitreal administration. In both cases the doses are high and surrounding tissue may suffer from side effects. Additionally, frequent intravitreal injections are invasive and can cause vitreous hemorrhages, retinal detachment and endophthalmitis.15 Thus, the development of long-term drug-delivery systems for the posterior eye is of increasing interest. Intravitreal implants may be one solution to chronic drug administration as they can be loaded with a wide range of drugs and allow for single injection and long-term drug delivery to the posterior segment of the eye. Intravitreal implants are generally injected into the vitreous or sutured to the sclera. Several non-bioerodible intravitreal implants have been developed and are tested in clinical studies. IluvienTM (pSivida, Watertown, MA, US) is a rod-shaped insert that fits into a 25 gauge (G) injection needle for the treatment of diabetic macular oedema (DMO) and has been designed to deliver a low dose (0.2 μg/day) over a 24- to 30-month period.16 The NT-501 (Neurotech Pharmaceuticals, Cumberland, RI, US) consists of encapsulated human cells genetically modified to secret ciliary neurotrophic factor (CNTF) for the treatment of retinal degenerative diseases.17,18 It is surgically implanted into the vitreous through a scleral incision and anchored with a suture through a small titanium loop. The implant I-vationTM (SurModics, Eden Prairie, MN, US) consists of a titanium helix coated with triamcinolone acetonide (TA) for the treatment of DMO.18 OzurdexTM (Allergan, Irvine, CA, US) and DurasertTM (pSivida, Watertown, MA, US) are examples for bioerodible intravitreal inserts. OzurdexTM is used to treat DMO or RVO and is composed of a polymer (PLGA) to release incorporated dexamethasone over a duration of 4 to 6 weeks.18 The DurasertTM technology system is designed to be delivered to the subconjunctival space of the eye where it releases latanoprost for predetermined periods of time ranging from days to years.15 All of these intravitreal inserts lack the ability to move and, thus, are not specifically directed to a pathological site in the eye. Furthermore, the removal of the non-bioerodible implants often requires a vitrectomy, adding to the risk of complications. To overcome these drawbacks, the utilisation of mobile and controllable microrobots has been suggested as a platform for targeted drug delivery to the posterior eye without the need for vitrectomy. Guiding intravitreal inserts to the diseased area allows for much slower release of drugs while providing an equivalent dosage of medication due to the non-linear nature of Fick’s law of diffusion.
Magnetic Manipulation for Ophthalmic Microrobots
Recent emerging technologies have paved the way for magnetically guided tools for minimally invasive surgery. These tools allow for more flexibility, increased stability and precision and they minimise the risk of perforation of tissue.19–21 Typically, magnetically guided surgical systems comprise a tethered magnetic tool, such as a flexible catheter, in an externally applied magnetic field. During medical procedures magnetic tools can be precisely positioned by systems utilising permanent magnets22 or electromagnets,23 which generate controlled magnetic fields and magnetic field gradients. Moreover, magnetically guided untethered microrobots have been proposed as surgical tools and as platforms for targeted drug delivery in ophthalmic applications.24
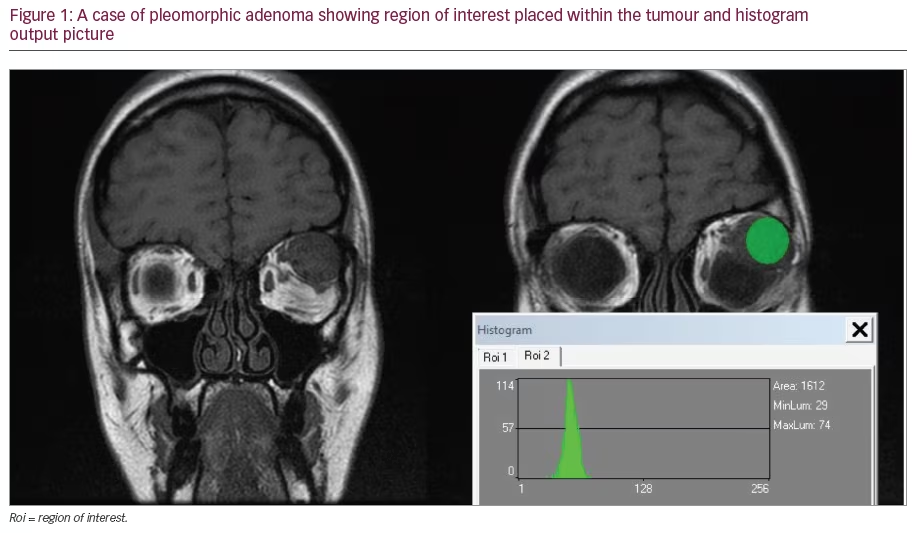
Microrobotic tools for sutureless ophthalmic surgery are rapidly gaining interest as in vivo diagnostic and therapeutic devices.25,26 In 1974, Charles D Kelman, better known for the development of phacoemulsification, first introduced the notion of the ‘phaco fly’, a wireless magnetic device that is slowly rotated in the capsular fornices to disrupt the cortex during cataract surgery.27 Intravitreal injection of a silicone magnetic fluid that incorporates ferromagnetic nanoparticles was suggested as a tamponading agent to alleviate retinal detachments and other types of retinopathy.28,29 During in vitro experiments the ferromagnetic fluid was injected into a model eye placed in a magnetic field, so that the nanoparticles interstitially diffused towards the magnetic source. Recent work shows the actuation of a single-hinged microswimmer, the ‘microscallop’, which can swim through non-Newtonian media.30 Propulsion of the structure was achieved in hyaluronic acid, one of the components of the vitreous humor, and thus shows potential for drug delivery in the eye, although the work did not consider the heterogeneous collagen fibre network as an obstacle. In 2010 Kummer et al. proposed an electromagnetic system for guidance of wireless microrobots inside the vitreous humor in the eye, called OctoMag.31 The system consists of eight electromagnets with soft-magnetic cores in a hemispherical arrangement with a central workspace of 20 x 20 x 20 mm, which approximately fits a human eye. A computer controls the amount of current in each coil and, thus, monitors the generated magnetic fields and gradients that are generated. The system, shown in Figure 1A, applies magnetic fields up to 40 mT and magnetic gradients up to 1 T/m to a magnetic device in the central workspace. The workspace is observed through an ophthalmic microscope equipped with a charge coupled device (CCD) camera and a wide field enhanced BIOM® lens for wide-angle imaging of the retina. Figure 1B illustrates the fast decay of magnetic field with increasing distance from the central workspace. At a distance of 300 mm from the central workspace, which is approximately the distance between the eye and heart, the magnetic fields have decreased to approximately 5 % of the applied field magnitude. The system provides high precision in medical procedures in a minimally invasive manner and allows for force feedback below the human force perception threshold. The OctoMag is teleoperated, potentially allowing surgeons to operate on patients remotely.
Patient Safety
Utilising magnetic fields and gradients for surgery has gained increasing interest in the medical community due to patient safety considerations. Several electrically assisted methods to optimise drug delivery have been suggested, such as ultrasound, electroporation32,33 or photodynamic therapy,34 whereas magnetic fields have been shown to penetrate deeply into human tissue while being very safe.35–37 The high degree of patient safety in magnetic fields arises from the small value of magnetic susceptibility of biological tissue.
The magnetic manipulation system, OctoMag, used for medical procedures in the eye, generates magnetic fields up to 40 mT, which is about one hundredth of the fields generated in a conventional magnetic resonance imaging (MRI) scanner and 200 times lower than the maximum suggested safe magnetic field strength for an adult human being.38 Moreover, the magnetic fields in the OctoMag decrease rapidly with increasing distance from the central workspace (as illustrated in Figure 1B). Minimally invasive microrobots for intraocular drug delivery or surgery have been proposed that have a cylindrical shape with an outer diameter of 285 μm and fit into a 23 G injection needle for a single injection into the patient’s eye without suture.39 The microrobots are rendered non-toxic by using biocompatible bulk materials and/or polymer or metal-based coatings.40 Smaller incisions in the eye attribute for faster recovery, less scarring and fewer complications during procedures and, thus, lead to improved patient safety.
Teleoperated Surgery
The first robot-assisted surgical procedure that was carried out from a distance, i.e. telesurgery, was reported in 2001 by Marescaux et al.41 Teleoperated robot-assisted microsurgery can decrease the fatigue an ophthalmic surgeon experiences after several hours of surgery. Furthermore, the use of teleoperated systems reduces the personnel and infrastructure required in an operation theatre and, thus, potentially lowers the cost of healthcare. Patients, as well as doctors, benefit from the ability to perform surgical procedures from a distance, which enables specialist surgeons to provide help to patients living in remote areas with limited access to healthcare without having to travel, thus, overcoming geographical constraints.
Like most magnetic manipulation systems, the OctoMag can be teleoperated via a computer. The graphical user interface allows the ophthalmic surgeon to choose the mode of input. The doctor chooses between manual control, which implies steering an intravitreal microrobot with a joystick, and automated control, where the integrated controller moves the microrobot on a predefined path. All surgical data are processed automatically and can be stored for future use. Furthermore, a surgeon’s movement and technique can be recorded for teaching lessexperienced surgeons or the system itself.
High Precision
Currently, no commercially available intravitreal insert used for drug delivery to the posterior eye has the ability to be directed to the pathological site and target it directly without affecting healthy surrounding tissue. Furthermore, the removal of many non-bioerodible inserts requires a vitrectomy thus adding further risk of complications. Using magnetically controlled microrobots to deliver drugs to a targeted site inside the eye shows great potential to decrease the required dosage while maintaining the same concentration of medication at the diseased area due to the nonlinear nature of Fick’s law of diffusion, which states that the concentration is highest closest to the source. By magnetically guiding a drug-loaded microrobot to a pathological site directly, the precision of drug delivery can be increased dramatically, thus, effecting healthy tissue less.
Furthermore, the trend in surgical ophthalmology is towards minimally invasive procedures and smaller instruments. Controllable intravitreal microrobotic tools allow for future sutureless ocular surgery. The small size of these tools can gain access to small organs and structures in the body and allows for better accuracy of surgical procedures. The precision of an ocular microrobot that is magnetically controlled inside the vitreous humor depends mainly on the camera resolution and the magnification of the ophthalmic microscope. The magnetic actuation system places no constraints on the position precision of the ophthalmic microrobot.
Force Feedback
Studies have shown that roughly 75 % of all forces applied during ophthalmic procedures are 7.5 mN in magnitude or lower, and less than 20 % of these forces could be felt by a surgeon5 and, therefore, lie below the human force perception threshold. Hence, in many cases ophthalmic surgeons are not able to feel interactions between a tool and the delicate tissues in the eye and, therefore, require significant levels of training, dexterity and experience. An electromagnetic manipulation system, such as the OctoMag, allows for direct force and torque feedback from the applied magnetic fields and gradients if the magnetisation of the microrobotic tool is known. The force F in [N] that an untethered microrobot applies to tissue can be derived as a function of the applied magnetic field gradients and the total microrobot magnetisation M according to where B is the magnetic field in [T]. The torque T in [Nm] that a microrobot applies to surrounding tissue is similarly calculated to give Restriction of the applied forces and torques by an upper threshold minimises the risk of damaging the delicate tissues in the eye, thus, increasing patient safety.
Microrobotic Applications in the Eye
Magnetically controlled microrobots can be used for various ophthalmic procedures, both in the anterior and in the posterior eye. Automated capsulorhexis has been presented as an example for a magnetically guided tethered microrobot application in the anterior eye. Untethered microrobots have been controlled in the posterior eye segment as diagnostic and therapeutic devices.
Anterior Eye
A hybrid magnetic-mechanical manipulation system for automated capsulorhexis utilising a flexible catheter with a sharp edge magnetic tip has been proposed.42 Capsulorhexis is one of the main steps in cataract surgery and describes the process of creating a circular hole in the lens capsule (as shown in Figure 2A). During this procedure, size, shape and location of the hole are crucial for later positioning of an artificial lens (intraocular lens [IOL]). A sharp edge magnetic blade is fixed on the distal tip of a flexible catheter with diameter of 600 μm (see Figure 2C). A piezoelectric actuator governs the longitudinal motion of the catheter with variable stepsize in the range of 10 to 100 μm. The lateral motion of the magnetic tool is controlled by the electromagnetic actuation system, OctoMag. The setup is illustrated in Figure 2B. The catheter tip is inserted into the anterior chamber of the eye through a small incision and anchored in the cornea with a trocar. The catheter tip is tracked visually and controlled, such that the combination of lateral and longitudinal motion allows it to follow a circle. Additionally, a force is applied downwards to insert a cut in the lens capsule tissue. During in situ experiments the precision and repeatability of the system were tested resulting in mean radial accuracy of 136 μm and standard deviation of 18 μm. Figure 2D shows a graph of the path followed by the catheter tip and compares it to the targeted circle.
Posterior Eye
Researchers have demonstrated an arrangement of two permanent magnets that can be used to magnetically inject therapeutic nanoparticles.43,44 This system has been used to overcome the blood– ear barrier in the inner ear in in vivo experiments by pushing magnetic nanoparticles with magnetic gradients. Furthermore, magnetic gradient based pulling of magnetised rat mesenchymal stem cells (MSC) has been used to selectively accumulate these nanoparticles at specific sites on the retina after intravitreal or intravenous delivery of MSC.45 In vivo experiments in rats showed that an orbital permanent magnet resulted in significantly higher concentrations of nanoparticles at the outer retina. Using magnetic gradient-based pulling or pushing mechanisms allows for high forces and increases accumulation of nanoparticles at specific sites and, therefore, could potentially be used in targeted drug delivery.
Untethered microrobots are larger compared with nanoparticles and can carry significantly larger amounts of drugs. Additionally, they can be observed and precisely manipulated during a medical procedure. Utilising an electromagnetic system, magnetic fields and gradients can be adjusted in the central workspace without moving the outer magnets but by simply controlling the currents in the coils. Wirelessly controlled microrobots have been suggested as platforms for targeted drug delivery in ophthalmic applications, such as the treatment of AMD. A hollow cylindrical microrobot has been developed with a drug reservoir. By directing the microrobot very close to a pathological site in the eye, the drug concentration at the targeted site can be very high while surrounding healthy tissue is unaffected. In order to bring the microrobot close to a targeted site, algorithms have been developed that allow it to follow a 3D path inside a model eye.46 The path that the microrobot follows can be pre-determined by the user, as seen in Figure 3A. The intravitreal microrobot is tracked with a camera and computer vision algorithms. An integrated closed-loop controller uses this information and adjusts the magnetic fields and gradients such that the microrobot follows the path. Magnetically steerable microrobots, equipped with small needles as illustrated in Figure 3B, have been used to puncture single veins on chorioallantoic membrane (CAM) of developing chicken embryos as a model for retinal veins.24 The advantages of utilising microrobots for these delicate procedures are the high precision of the injection and force feedback in real-time during the puncture event.
While intravitreal microrobots show great potential as a platform for targeted drug delivery and as assistive tools for precise ophthalmic surgery, they can also be utilised as diagnostic tools. A luminescence oxygen sensor has been integrated with an intraocular microrobot to sense oxygen concentration in the vitreous.47 The minimally invasive microrobot is coated with Pt(II) octaethylporphine dyes as luminescence material and polystyrene as a supporting matrix. In the presence of oxygen in the vitreous the porphine dyes are quenched. This process decreases the emission lifetime and intensity, indicating the concentration of oxygen in the eye.
After a microrobot-assisted procedure has been finished, the microrobot is removed from the vitreal chamber with the aid of a customised magnetic tool. The tool consists of a magnetic wire that is inserted into a 23 G injection needle and attracts the magnetic microrobot. When the microrobot attaches to the magnetic wire it can be pulled into the injection needle and removed from the eye.
In vivo Applications of Microrobots in the Lapine Eye
Mobility and controllability of magnetically guided untethered microrobots inside a living eye were investigated.39 In vivo studies were conducted in five individual New Zealand White rabbit eyes, three of which were vitrectomised and subsequently filled with silicone oil (viscosity 1,000 mm2/ second at 25°C) or balanced salt solution (BSS). A cylindrical microrobot with outer diameter of 285 μm was injected into the vitreal chamber, which was filled with vitreous, silicone oil or BSS, with a 23 G needle for sutureless injection as shown in Figure 4B. The anaesthetised rabbit’s head was placed in the central workspace of the OctoMag system, illustrated in Figure 4A. The electromagnetic manipulation system was then used to rotate and translate the intravitreal microrobot inside the eye with various rotation frequencies, magnetic field magnitudes and magnetic gradients. It was shown that minimally invasive microrobots feature good 3D mobility and allow for rotation and translation inside the eye (see Figure 4C). Experiments show that intravitreal introduction of wirelessly controlled microrobots can enable sutureless and precise ophthalmic procedures in several surrounding media, such as vitreous, silicone oil and BSS.
Biocompatibility and Functional Coatings for Ophthalmic Microrobots
A parallel area of research in the field of ophthalmic microrobotics deals with the definition of materials and fabrication strategies that can enhance the biocompatibility and the functionality of the microdevices. A common strategy to address the challenges related to the interaction with the biological environment is to implement surface coatings on magnetic microcarriers with different shapes and sizes. Figure 5A shows three differently coated and shaped microdevices for ophthalmic applications. A scanning electron microscopy (SEM) image of a hollow microdevice with a lumen for enhanced drug-loading capabilities is shown in Figure 5B. Appropriate surface properties are essential in terms of contact of the microrobots with cells or body fluids, as well as to limit any foreign body reaction that would inhibit the functional activity of the implant.48,49
Polypyrrole (PPy) is one of the most widely researched conductive polymers because of its mechanical stability, ease of synthesis and deposition processes. Its intrinsic biocompatibility is also an important quality that makes PPy coatings ideal for biomedical applications. Recently, PPy layers were proposed as drug-delivery coatings on ophthalmic microrobots50 and fabricated by means of electrodeposition. Studies with small ionic drug models have shown the possibility to provide a diffusion driven release for a few hours with only 6 μm thick deposits. Drug loading, kinetics behaviour and biocompatibility were found to be modulated and tailored by fabrication parameters, such as the type of electric signals used for the deposition, the inclusion of dopants51 or the preparation of multilayers.
Chitosan is a polysaccharide derived from naturally available chitin, which has been proposed for medical applications in the eye, because of its biocompatibility, biodegradability, low cost and its bioactive properties as a penetration enhancer.52,53 Its polymeric structure characterised by the presence of primary amine groups allows the formation of pH-responsive hydrogel films by application of negative electric signals on conductive surfaces. A microrobot coated with chitosan is depicted in Figure 5C. The method has been proposed to create long-term responsive drug delivery coatings on ophthalmic microrobots,54 with drug loading similar to commercial implants. A model drug could be released by simple diffusion in a time frame of a month, or with accelerated kinetics by means of a slight decrease of pH as accompanies inflamed or diseased tissue.55,56
These examples are only two possible scenarios related to the functionalisation of ophthalmic microrobots. Material science and micro fabrication expertise can provide many other alternative coatings depending on the desired procedure and requirements.
Conclusion
Technology for ophthalmic applications is advancing quickly. Various assistive robotic systems for ophthalmic surgery are under development to overcome human tremor and limitations of perception. Furthermore, several bioerodible and non-bioerodible inserts have been suggested for drug delivery to the posterior eye. However, the drawback of these structures is their passivity and the inability to control their motions. Ocular microrobots that can be guided wirelessly by externally applied magnetic fields and gradients show great potential for targeted drug delivery in the eye and as assistive tools for ophthalmic surgery. The use of these structures, which are guided by magnetic manipulation systems, allows for high patient safety due to the deep penetration and safety of magnetic fields and the minimally invasive nature of the procedure. The manipulation system, OctoMag, is teleoperated and can be operated in manual mode or automatically, with an integrated controller. Due to the small size of the microrobot and the high resolution of its movements, the spacial precision reached is high. Real-time force feedback is given to the operator to restrict applied forces and decrease the risk of damaging the delicate tissues in the eye.
Magnetically actuated systems have been suggested to assist in applications in the anterior and the posterior eye and can guide tethered as well as untethered structures. A magnetic-mechanical hybrid actuation system for high-precision capsulorhexis utilising a flexible catheter has been introduced to aid in minimally invasive cataract surgery. In the posterior eye, wirelessly controlled microrobots can be guided precisely on a predefined path and their mobility and controllability have been successfully demonstrated in in vivo studies in the living lapine eye.