Blepharoptosis is a common complication following eye removal.1 Blepharoptosis in acquired anophthalmia can exacerbate a pre-existing sense of facial deformity and dissatisfaction.2 In many patients, a favourable cosmetic outcome can be achieved without further surgery. Augmentation of the superior aspect of the prosthesis can mechanically elevate or vault the upper eyelid. However, this may be limited by other complications, including lower-eyelid retraction, hypoglobus and loss of motility.3,4
Rehabilitating the anophthalmic socket includes augmenting orbital volume, which may be achieved by modifying the prosthesis.5 A thicker prosthesis often independently elevates the upper eyelid through posterior support. Yet, prosthesis thickness inversely correlates with motility.6 In addition, prostheses that are thick or heavy may compromise other aspects of fit, including causing a hypoglobus appearance or lower-eyelid retraction, or both.7 Volume deficiency may be surgically treated by inserting autologous or alloplastic orbital implants.8–10 Vistnes suggests that upper-eyelid blepharoptosis should be corrected after addressing volume deficit.1
This article reviews the pathophysiology and treatment of blepharoptosis in anophthalmia, and describes a novel technique and the use of a limbal demarcated template prosthesis to facilitate levator resection surgery and optimize prosthesis fabrication processes.
Methods
Literature review methodology
This is a review of the literature and a retrospective chart review. The authors searched the PubMed database in October 2021 for “anophthalmic” or “anophthalmia” or “anophthalmos” and “ptosis” or “blepharoptosis”. The search was limited to studies in English, yielding 71 articles. From these, the references were reviewed for pertinent articles addressing blepharoptosis in an anophthalmic socket. Reviews, book chapters and editorials were excluded, as were articles describing transient eyelid elevation with pharmacologic agents or lid crutches. Thirteen original articles were reviewed in their entirety.
Chart review methodology
Charts of patients with blepharoptosis in the setting of ipsilateral anophthalmia were reviewed. Only cases with adequate orbital volume and levator function, and without cranial neuropathy, were included retrospectively. The included patients were treated using the following surgical technique.
Surgical technique
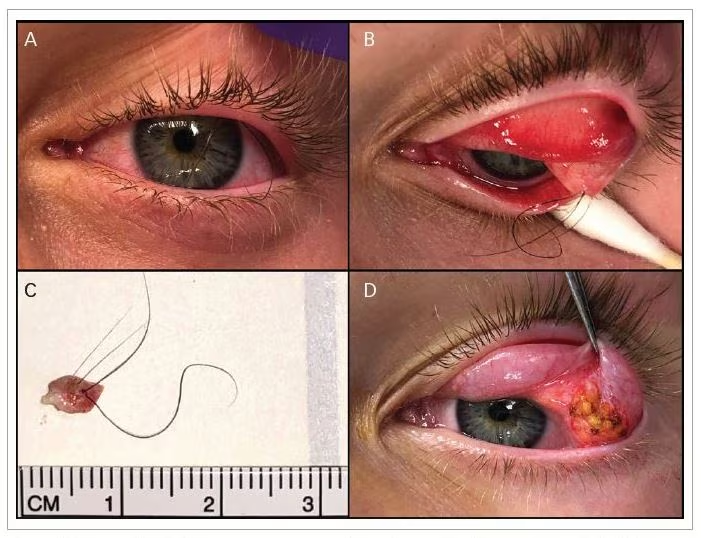
A preparatory prosthesis with the limbus demarcated was prefabricated prior to surgery. The prosthesis was customized in size, contour and thickness as the final planned prosthesis (Figure 1A). The temporary prosthetic shell was configured to fit well into the anophthalmic socket, with desired margin to reflex distance 2 (MRD2; light reflex to lower eyelid margin) and volume, yet without attention to the MRD1 and without any attempt to address blepharoptosis mechanically. In other words, the ocularist was asked to fit the temporary prosthesis without augmentation or vaulting techniques that normally raise the upper-eyelid margin. An outline of the limbus was rendered on the shell that otherwise was not detailed.
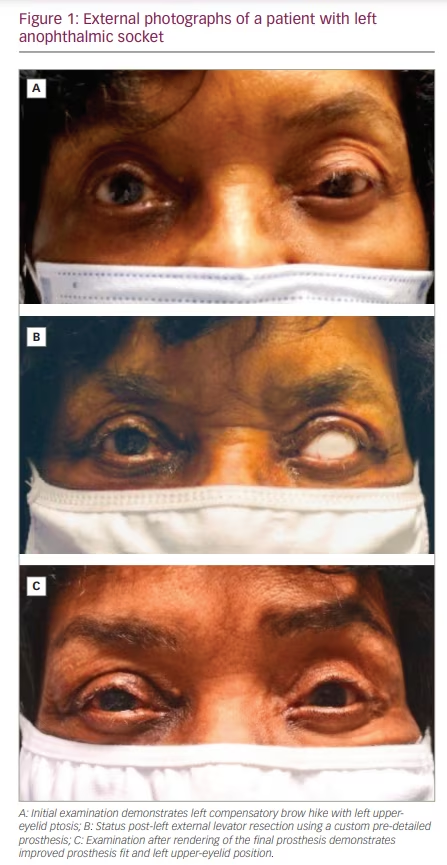
Under light sedation or not, the upper-eyelid crease was marked, and the upper eyelid was infiltrated with 3 mL of 1% lidocaine with 1:100,000 adrenaline combined with 0.5% bupivacaine and sodium bicarbonate in a 4.5:4.5:1 ratio. With the template prosthesis underneath the eyelid, a small amount of skin and underlying orbicularis and pre-aponeurotic fat was excised in a blepharoplasty fashion. The levator aponeurosis was exposed and resected between 3 and 10 mm, depending on the amount of desired upper-eyelid elevation. The aponeurosis was secured to the upper anterior tarsal border using 2 or 3 interrupted 7-0 silk sutures. Adjustments were made using the limbal marking as a landmark for eyelid contour and positioning (Figure 1B). After surgery, the ocularist made final adjustments as well as renderings of iris and scleral detail to the prosthesis (Figure 1C).
Charts were reviewed for MRD1, symmetry, prosthesis fit and motility at a minimum of 6 months’ follow-up. The need for revision surgery or additional prosthesis fabrication was recorded.
Results and discussion
Literature review on pathophysiology and special considerations in an anophthalmic socket
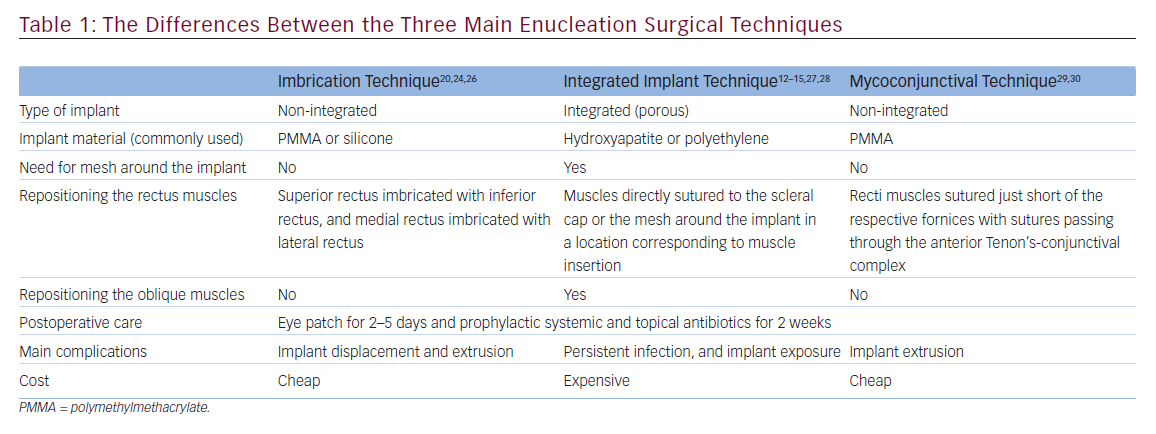
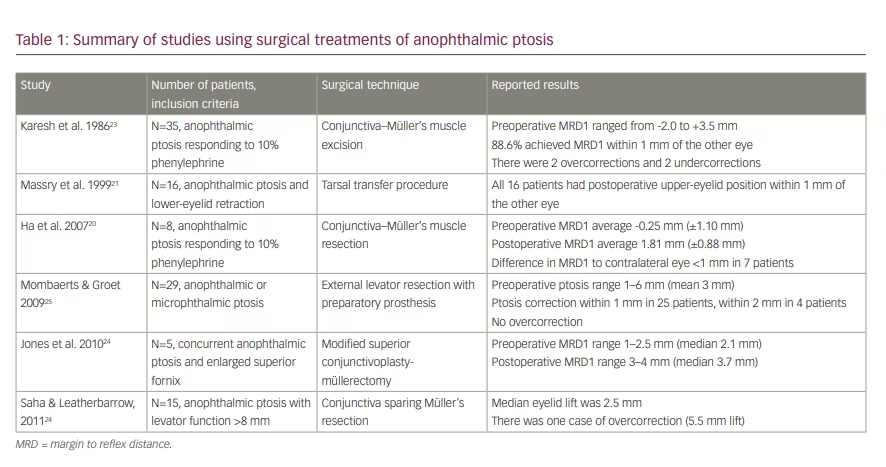
Four articles investigated the pathophysiology of ptosis in anophthalmia, six reported surgical techniques used to treat anophthalmic blepharoptosis (Table 1) and three discussed treatments of blepharoptosis using prosthesis augmentation. Ptosis in an anophthalmic socket may arise from various factors, including volume loss, soft-tissue rotation, lower-eyelid laxity or socket fibrosis.11 In particular, orbital volume deficiency is important.1 Insufficient volume replacement can lead to post-enucleation socket syndrome (PESS), characterized by fat atrophy, ptosis, deep superior sulcus and lower-eyelid laxity in an anophthalmic socket.3 Kaltreider et al. described a direct relationship between per cent volume-replacement remaining and the occurrence of ptosis. For patients with 40% volume replacement, the odds of ptosis were 2.27 times greater than patients with 80% volume replacement. Additionally, ptosis improved in 30% of patients after orbital volume replacement.12
Levator dehiscence or dysfunction is another pathophysiologic mechanism for blepharoptosis in anophthalmia. Vistnes reported ptosis in 18% of anophthalmic patients (n=66) despite an adequate prosthesis and adequate orbital volume. Vistnes attributed ptosis in these cases to an altered normal pivot point of the levator muscle and a subsequent mechanical imbalance.1 Another study of 32 patients showed levator function was significantly lower in anophthalmic orbits (mean 10.43 ± standard deviation 1.48 mm) than in contralateral normal orbits (mean 12.74 ± standard deviation 1.81 mm).13 Levator function also correlated with height of prosthesis, and was highest with a prosthesis of proper height. Additionally, levator function in anophthalmic orbits directly correlated with increased anterior projection of an implant and with larger implant size, and inversely correlated with age and superior sulcus deepening.14
Non-surgical techniques in the literature
In a review of 186 patients who underwent enucleation, Verhoekx et al. found that 62.3% of postoperative complications could be managed conservatively with an adjustment to the prosthesis.10 Prosthesis adjustments, by adding volume or changing the shape, can correct mild upper-eyelid ptosis and lead to a satisfactory outcome in most cases.10,15 A ptosis crutch or shelf can be mounted on spectacles or fabricated onto the prosthesis.16,17 The superior aspect of the prosthesis can be cut to form a shelf for the upper eyelid to rest.18 However, this can increase the weight of the prosthesis and potentially limit motility, though this was not assessed by these studies.
There is an upper limit of weight beyond which prosthesis augmentation causes downward displacement of the lower lid and orbital tissues. In a case series of 70 patients, Kaltreider found the volume supplied by ocular prosthesis ranged from 0.75 mL to 4.2 mL.4 The smaller prostheses were associated with implant malposition and socket contraction, while larger prostheses were associated with ptosis and lower-eyelid laxity. Kaltreider suggested an ideal prosthesis volume of 2.2 mL with an upper limit of 4.2 mL. Careful selection and adjustment of the ocular implant is necessary for a desirable cosmetic outcome.4
Surgical techniques in the literature
In the case series by Verhoekx et al., blepharoptosis was the most common postoperative complication of enucleation, requiring surgery in 7% of patients.10 The consensus in the literature is that surgical repair of upper-eyelid ptosis in anophthalmia should be addressed after addressing volume deficit and lower-eyelid malposition.1 While prosthesis augmentation can add volume or elevate the eyelid margin, it usually compromises prosthesis fit and motility.17 Hence, surgical volume expansion of the deeper orbit may be indicated. Sendul et al. described 12 out of 18 patients in whom blepharoptosis was improved after volume replacement with a dermis fat graft.19 The remining 6 patients required subsequent eyelid ptosis repair surgery.
Surgical techniques for upper-eyelid ptosis repair in anophthalmic sockets include levator resection, tarsal switch and conjunctiva–Müller’s muscle resection (Table 1).9,11,20–23 Levator resection with an external approach was the most common method for correcting ptosis in anophthalmia. However, an internal approach has also been described.20,22–24 Karesh et al. treated 35 patients with anophthalmic ptosis that responded to 10% phenylephrine with a conjunctiva–Müller’s muscle resection. Overall, 31 eyelids achieved a postoperative level within 1 mm of the opposite eyelid, 2 were overcorrected and 2 were undercorrected. None of the patients had complications of the superior fornix, including socket dryness or inability to retain the prosthesis.23 Jones et al. used a superior conjunctivoplasty-müllerectomy to correct ptosis and enlarged superior fornix with chronic discharge in five anophthalmic patients. All patients reported subjective improvement in discharge and MRD1 improved from a median of 2.1 mm preoperatively to 3.7 mm postoperatively.22
Massry et al. used a tarsal switch technique to treat 16 patients with anophthalmic ptosis and lower-eyelid retraction.21 The technique consists of an upper-eyelid tarsectomy with transfer of autologous tarsoconjunctival graft to the posterior lamella of the lower eyelid. The average preoperative ptosis was 3.7 mm, while the average postoperative ptosis was 0.4 mm. All 16 patients had a postoperative eyelid position within 1 mm of the fellow eye. Two patients were overcorrected within 1 mm and eight patients were undercorrected within 1 mm. This technique confers the advantage of addressing upper- and lower-eyelid malposition simultaneously but may be limited by the amount of donor tissue available.19
Mombaerts and Groet described a technique using a debulked preparatory prosthesis aimed at vertically aligning the pupils without any ptosis correction (i.e. volume reduced at the superior aspect). They report 29 patients with severe upper-eyelid ptosis who underwent levator aponeurosis surgery via an anterior approach and in the setting of the preparatory prosthesis.25 They achieved a satisfactory result (1 mm residual ptosis or less) in 25 of 29 patients (86%) and an unsatisfactory result (2 mm of residual ptosis) in the remaining 4 patients, without any cases of overcorrection. After surgery, 24% of patients required volume augmentation to the preparatory prosthesis to correct residual pupil displacement or ptosis.
Chart review results
We reviewed the results of 12 anophthalmic patients with adequate orbital volume who underwent external levator surgery repair using a preparatory prosthesis with limbus demarcations and with final prosthesis modifications post-surgery. At a minimum 6-month follow-up, 12 patients achieved MRD1 within 1 mm of the contralateral eye with no loss of motility or other compromise to prosthesis fit.26 In all patients, symmetry contour and height of the eyelid margin was satisfactory to the patient and the surgeon. At a mean follow-up of 3 years, no additional surgery or prosthesis adjustment was necessary.24
Conclusions
The pathophysiology of blepharoptosis following eye removal is often due to inadequate orbital volume. The literature consensus is that orbital volume is an important variable in ptosis in an anophthalmic socket; in many cases, treating orbit volume corrects upper-eyelid malposition.
While volume replacement through prosthesis modification may elevate the upper eyelid, it may compromise other aspects of prosthesis fit or motility. Adjusting the ocular prosthesis and using other non-surgical approaches may result in satisfactory outcomes in many cases.
In cases requiring surgical intervention, techniques corresponding to non-anophthalmic ptosis repair have been reported. Collaboration between the ocularist and eyelid surgeon is important. The use of a prosthesis fitted for the socket, except for upper eyelid ptosis, may optimize the efficiency of ptosis repair surgery compared to traditional methods where the surgery and prosthesis fittings are often done sequentially and independently. The authors’ findings corroborate Mombaerts and Groet who described the use of a preparatory, eye image detailed prosthesis absent of a ptosis-correcting superior vault.
Our use of a custom prosthesis with only limbal tracings may have the advantage of requiring fewer device modifications. The preparatory prosthesis method Mombaerts and Groet described was associated with 24% needing ocularist modifications. Our technique of performing levator resection surgery prior to final prosthesis fabrication allowed high precision and obviated prosthesis refabrication or repeat surgery in this series.
All the studies we reviewed were retrospective and limited by a small sample size. The various techniques have not been directly compared. Prospective controlled studies may elucidate the comparative efficacy of the various treatment options.