Uveal melanoma is the most common intraocular primary malignancy. The incidence is reported to be four to seven per million per year in the Caucasian population. Patients usually present around the fifth or sixth decade of life; however, this tumor can rarely occur in young children. The large majority of patients are Caucasian, with this malignancy rarely occurring in Hispanics, Asians and African-Americans.1 There is no sex preponderance. Risk factors for uveal melanoma include fair skin, light-colored eyes, melanocytoma, congenital ocular melanocytosis and neurofibromatosis.
Presentation and Diagnosis
Patients usually present with visual symptoms such as metamorphopsia, blurred vision, photopsia and visual field loss. A significant minority are asymptomatic and detected on routine examination.
Clinical diagnosis is mostly based on indirect ophthalmoscopy combined with ultrasonography and, in selected cases, biopsy.2 Misdiagnosis is rare in specialist centers. Small melanocytic tumors of uncertain malignancy tend to be observed for tumor growth. Shields et al. have described clinical risk factors for growth and metastasis.3–5
Traditionally, uveal melanoma has been classified as small (less than 3mm in thickness), medium (3–10mm in thickness or up to 15mm in basal diameter), and large (more than 10mm in thickness or more than 15mm in basal diameter).
Ocular Treatment
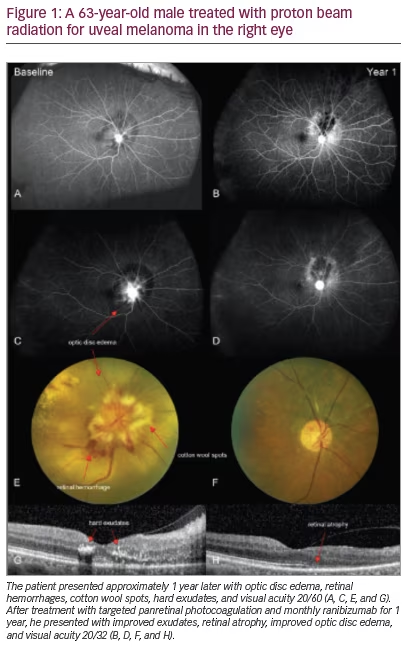
Treatment is based on tumor size and location, visual acuity, status of the fellow eye, and the patient’s fears and wishes.6 Treatment options for uveal melanoma include brachytherapy, proton beam therapy, stereotactic radiotherapy, trans-scleral local resection, transretinal endoresection, transpupillary thermotherapy, and enucleation. In most centers, the first choice of treatment is brachytherapy, using either an iodine-125 or ruthenium-106 plaque. Proton beam radiotherapy is available only in a few centers, where it is used either in all patients (e.g. Boston) or in selected cases, when brachytherapy is not appropriate (e.g. Liverpool). There is growing interest in stereotactic radiotherapy in centers where proton beam radiotherapy is not available. Trans-scleral local resection is widely practiced for small iris and ciliary body tumors but performed by only a few surgeons as a treatment for large, choroidal melanomas. Transretinal endoresection is controversial because of concerns that piecemeal tumor removal might disseminate malignant cells around the eye and systemically; it is therefore performed only when it offers the only hope of conserving useful vision. Transpupillary thermotherapy and photodynamic therapy can be successful with small tumors, but are less reliable than radiotherapy and therefore administered only in selected cases (e.g. elderly patients with diabetes mellitus). Increasingly, different therapeutic modalities are being combined to enhance local tumor control while minimizing ocular morbidity. Procedures such as secondary local resection, transpupillary thermotherapy, photodynamic therapy, sector laser photocoagulation, subtenon injections of steroids and intraocular injection of antiangiogenic agents might reduce radiation-induced complications.7 There is a growing realization that much ocular morbidity after radiotherapy is caused by the persistence of bulky, necrotic tumor.
Estimating the Prognosis for Survival
Despite good local tumor control, about 20–50% of patients die of metastatic disease within 10 years. Metastatic disease almost always involves the liver and is usually fatal within a few months.8 Factors indicating a poor prognosis include: increased patient age; larger tumor size, both with regards to diameter and thickness; ciliary body involvement; epithelioid cell type; extraocular extension; lymphocytic infiltration; high mitotic rate; and loss of chromosome 3. Metastatic death occurs almost exclusively in patients with a monosomy 3 melanoma, which is almost always fatal.9
The highly predictive nature of monosomy 3 loss has encouraged more ocular oncologists to offer cytogenetic tumor typing to all patients with uveal melanoma, performing biopsy in patients treated by radiotherapy.10,11,14–16 However, there are several controversial points related to this practice. First, there are concerns about sampling errors, so that lethal mutations are not detected. Second, there is uncertainty about the impact of an adverse prognosis on quality of life, especially as it is rare for any treatment to prolong life.17,18 Cook et al. have shown that concerns about psychologic harm are exaggerated. Third, there are several chromosomal abnormalities other than monosomy 3 that are known to correlate with prognosis (e.g. chromosomes 6, 8, 15 and 18), but it is not known how best to use this information.19
Harbour et al. have classified uveal melanomas as being of class 1 and class 2, these having a low risk and a high risk of metastasis, respectively.20,21 Landreville et al. described molecular features of metastasizing and non-metastasizing uveal melanomas. As an example, gaining of chromosome 6p tends to occur in non-metastasizing, disomy 3 tumors whereas monosomy 3 is present in metastasizing tumors. Landreville et al.21 suggest that gains in chromosome 6p and monosomy 3 are mutually exclusive, but this is not always the case. Using gene expression profiles, they described four subgroups, with increasing risk for metastasis: Class 1A, with the longest metastasis-free survival and minimal aneuploidy; Class 1B: gaining of 6p; Class 2A: monosomy 3; and Class 2B: monosomy 3 and 8p loss, highest risk for metastatic disease.
It seems that class 1 tumors represent normal uveal melanocytes whereas class 2 tumors show a relative blockage for melanocytic differentiation so that they resemble neural and ectodermal stem cells.
Damato et al. have emphasized the importance of combining genomic tumor type with clinical tumor stage and histologic grade of malignancy, which indicates how long any metastases are likely to have been present and how fast they are growing.11 Such multivariate analysis is further enhanced by taking normal life expectancy based on age and sex into account.
Prognostic Tumor Biopsy
Different biopsy techniques have been described. These include fine needle aspiration biopsy, performed either transvitreally or transclerally, and biopsy with a 25-gauge vitrector.12–14 Chromosome 3 status was successfully determined in 86% of patients who underwent fine needle aspiration biopsy, in the experience of Shields et al. the only complication described in their article was minimal transient vitreous hemorrhage at the tumor biopsy site, when the biopsy was performed transvitreally (almost 50%).14 With brachytherapy the biopsy is carried out immediately before the radioactive plaque insertion whereas with proton beam radiotherapy some practitioners delay biopsy until the radiotherapy is completed, to minimize any risk of tumor seeding.14,15 If possible, multiple tumor sites are sampled because some tumors are heterogenous, with monosomy 3 being confined only to some parts of the tumor.
Impact of Ocular Treatment on Survival
The Collaborative Ocular Melanoma Study (COMS) Group have performed randomized trials investigating the impact of brachytherapy and pre-enucleation radiotherapy on survival in comparison with enucleation alone; however, these studies lacked sufficient statistical power because many patients that were enrolled were likely to have had a non-lethal melanoma.6,22 The COMS study on small choroidal melanomas (report No. 4) suffered from the same shortcoming.23,24 It would be ideal if further randomized studies could be performed to determine the impact of ocular treatment on survival; however, any future clinical trials investigating the influence of ocular or systemic treatment on survival should take account of tumor lethality determined by genomic tumor type. Robertson has emphasized the difficulties of performing multicenter, randomized studies because of the largenumbers of patients required.18 With genomic tumor typing and improved prognostication it may be possible to achieve sufficient statistical power for such studies with fewer patients.
Genomic tumor typing and improved statistical methods have enhanced our understanding of uveal melanomas and their natural history.23 There is growing evidence that metastatic spread occurs at a very early stage at least in some tumors so that by the time the patient presents to an ophthalmologist any opportunities for influencing survival might have gone.8,25 It seems that in patients with medium-sized and large tumors, the scope of ocular treatment is only to conserve a comfortable eye with as much useful vision as possible. This realization opens the way for less aggressive ocular treatment with reduced ocular morbidity. With small choroidal melanocytic tumors, management is more controversial. Some advocate observation until growth is documented, in the hope of avoiding unnecessary treatment; others recommend early therapy, when any opportunities for preventing metastatic spread are greatest. It is relevant that monosomy 3 is present in at least 30% of patients with small melanoma.15
Screening for Metastatic Disease
Screening for metastatic disease is also a topic of controversy. This requires six- or twelve-monthly liver function tests and liver imaging; however, there is no consensus as to whether screening should be recommended to all patients or only those at high risk of metastasis.
Need for Systemic Adjuvant Therapy
With monosomy 3, or class 2, melanomas, the disease is no longer confined to the eye but is systemic and should be approached in that manner. The best hopes for prolonging life, therefore, lie with systemic adjuvant therapy. It is hoped that improved international communication and collaboration will make it possible for large, multicenter, randomized trials to investigate any promising therapeutic agents. It is likely that lethal uveal melanomas will show a variety of subtypes so that the key to success may well lie in personalizing treatment for each individual patient according to the cell signaling pathways that are abnormal.
Conclusion
One can only speculate as to when uveal melanomas start to metastasize. It is therefore not known whether ocular treatment influences survival and, if so, in whom. Many patients with uveal melanoma may be sacrificing vision and the eye unnecessarily in the forlorn hope of living longer. Methods for conserving the eye and vision have improved but, because of concerns about metastasis, are either not applied or are administered too aggressively. Randomized controlled trials evaluating the impact of ocular treatment on survival would require patients to be stratified according to genomic tumor type, that is, according to the lethality of their tumor. Proper clinical staging, histologic grading and genomic typing of tumors also enhance prospects for undertaking randomized trials evaluating novel agents for systemic adjuvant therapy.