Twenty-five percent of patients who visit ophthalmic clinics report symptoms of dry eye and it is one of the most common conditions seen by eye care practitioners.1 Approximately two-thirds of patients affected by dry eye disease (DED) are female and elderly,2,3 and there is a higher risk in postmenopausal women.4 The occurrence of severe forms of DED is reported to increase with age and almost 8% of women and 4% of men over the age of 50 years have more severe DED.5,6 The prevalence rates of DED have been shown to vary substantially across different geographical regions.7–13
Epidemiological studies of Indian populations report prevalence rates of 9.5–370/1,000 for psychiatric disorders.14 The chronic discomfort observed in patients with DED may also have a negative impact on other aspects of patient health, such as cognitive processes, mood and mental health.15 When quality of life is affected, a patient’s psychological wellbeing is also affected, leading to initiation of mental imbalance. Some psychological and mental health issues such as sleep disorders, anxiety, depression and mood disturbances have also shown to be triggering factors for DED,16,17 thus indicating a mutually reversible relationship between DED and mental health status. Additionally, drug intake for mental health disorders may contribute to DED.18
In recent years, a number of researchers from western countries have investigated the impact of DED on psychiatric wellbeing in large retrospective epidemiological studies.19,20 These studies, in general, have shown a positive association between DED and psychiatric comorbidities. Incidentally, there are almost no studies from developing countries, particularly India, on this issue. The purpose of the present study is to address the dearth of research on mental health status and DED in developing countries.
Material and methods
Study participants were split into two groups: those diagnosed with DED and a control group with no diagnosis or symptoms of DED. All observations were conducted at the Department of Ophthalmology, Era’s Lucknow Medical College, Lucknow, India. Exclusion criteria included DED due to ocular pathologies, hypertension, diabetes mellitus, dysthyroidism, smoking, any drug intake for more than 3 months and any radiation therapy or surgery in the past 3 months. Users of computers and smart phones for more than 8 hours daily were also excluded as device use can contribute to the development of DED and may confound the study.21,22 A detailed history regarding ocular symptoms, with emphasis on symptoms associated with DED, was obtained from all subjects included in the study. Informed consent was obtained from all study participants. Tear production grading and ocular symptoms were measured using three tests: Schirmer’s test, tear-film break-up time (TBUT) test and ocular surface disease index (OSDI).23,24
Schirmer’s test
A specialised Schirmer’s strip was prepared from Whatman™ filter paper (GE Healthcare Life Science, Chicago, IL, US) measuring 40×5 mm, graded 0–35 mm. A 5 mm strip was folded and placed in the lower fornix at the junction of medial 2/3 and lateral 1/3, and time noted. Extent of wetting of the strip was noted after 5 minutes. Wetting of less than 15 mm was regarded as effective tear production. Grading of tear production was as follows: normal = ≥15 mm, mild = 9–14 mm, moderate = 4–8 mm, severe = ≤4 mm.
Tear-film break-up time test
Fluorescein strip was used to stain the eye. The patient was asked to blink three or four times to distribute the dye in conjunctival sac and was then asked to look straight ahead and not to blink. The eye was scanned using slit lamp under cobalt blue light; the first area of tear film rupture, manifested by the appearance of a black island within the green film of fluorescein, was noted. TBUT was the time, in seconds, between the last blink and the appearance of a dry spot on cornea categorised as: normal = >10.0 seconds, mild = 6.1–10.0 seconds, moderate = 3.1–6.0 seconds, severe = ≤3 seconds.
Ocular surface disease index
OSDI measures the severity of DED (normal, mild to moderate and moderate to severe) based on a 12-item patient-reported outcome questionnaire. Grading is as follows: normal = 0–12 points, mild to moderate = 13–31 points, moderate to severe = 32–100 points.25
Evaluation and categorisation of mental health status
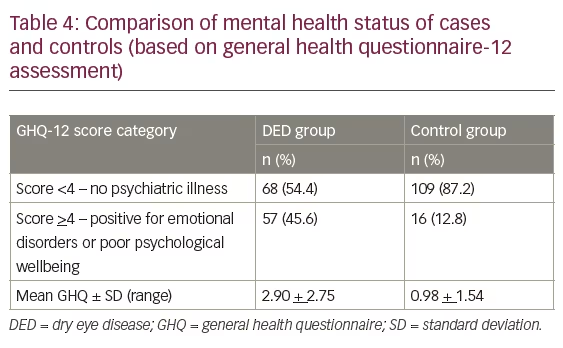
All study participants were subjected to general health questionnaire (GHQ)-12 to evaluate and categorise mental health status.26,27 A GHQ-12 score of ≤3 is considered normal, and these patients would require no further evaluation. A score of ≥4 is considered abnormal and requires further patient evaluation for psychiatric disorders.
Statistical analysis
The statistical analysis was done using SPSS (Statistical Package for Social Sciences) Version 15.0 statistical analysis software. The values were represented in number (%) and mean ± standard deviation (SD). Student’s t-test was performed to test the significance of two mean values. An a priori benchmark of statistical significance was set at p<0.05, with p<0.01 being highly significant and p<0.001 very highly significant.
Results
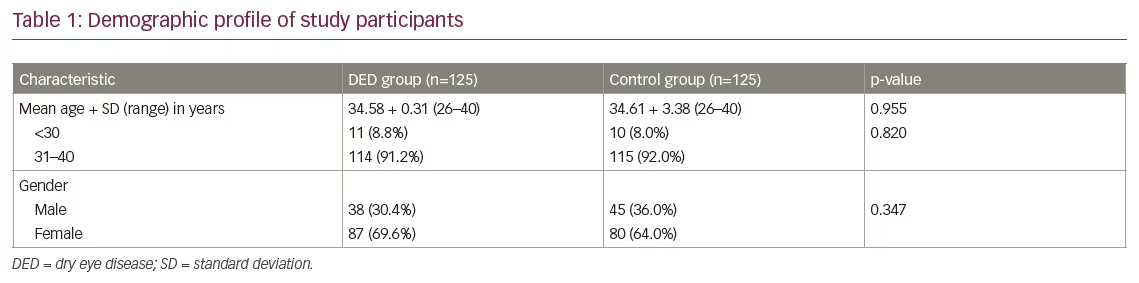
A total of 125 patients fulfilled the inclusion criteria and had a diagnosis of DED. Another 125 healthy volunteers were recruited as a control arm. The mean age was 34.58 ± 0.31 years in the DED group and 34.61 ± 3.38 years in the control group. There was no significant difference in age between the two groups (p=0.820). The majority of participants in the DED group, as well as the control group, were female (69.6% and 64.0%, respectively). There was no significant difference between the groups with respect to gender (p=0.347). Baseline characteristics are provided in Table 1.
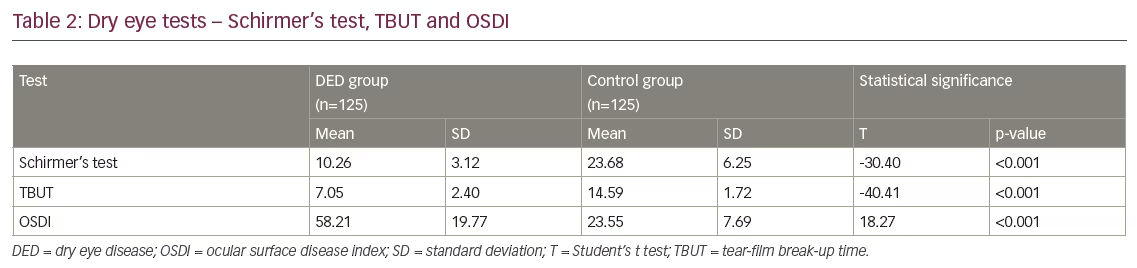
Mean values for Schirmer’s test and TBUT were 10.26 ± 3.12 and 7.05 ± 2.40, respectively in the DED group, and 23.68 ± 6.25 and 14.59 ± 1.72, respectively in the control group. Statistically, for both the parameters, there was a significant difference between the two groups (p<0.001). Mean OSDI values were significantly higher in the DED group (58.21 ± 19.77) compared to that of the control group (23.55 ± 7.69; p<0.001) (Table 2).
As per OSDI, only 6 (4.8%) participants in the DED group were in the normal range, 103 (82.4%) had mild to moderate OSDI grade and 16 (12.8%) had moderate to severe OSDI grade. In the control group, a total of 121 (96.8%) had normal and only 4 (3.2%) had mild to moderate
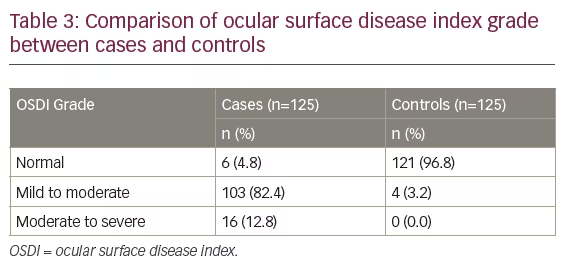
OSDI grade. Statistically, there is a significant difference between the two groups with respect to OSDI grade (p<0.001) (Table 3).
Using the GHQ-12 inventory a total of 57/125 participants in the DED group (45.6%) and 16/125 in the control group (12.8%) had scores of >4, indicating emotional disorders or poor psychological wellbeing (p<0.001) (Table 4). In the DED group, prevalence of psychiatric disorder was 23% for patients with mild DED, 97% for those with moderate DED and 100% for those with severe DED (based on Schirmer’s test). The incidence of psychiatric disorders was significantly higher for those with moderate and severe DED as compared to mild (p<0.001).
Discussion
In the present study, we made an attempt to evaluate the association between psychiatric disorders and the severity of DED. Using Schirmer’s test and GHQ-12 to quantify the severity of DED and mental wellbeing, respectively, we found that only 23% of patients with mild DED experience psychiatric comorbidity, whereas those with moderate and severe DED had a significantly higher risk of psychiatric comorbidity (97.0% and 100.0%, respectively). When looking at the DED group as a whole, the results presented here indicate a significantly higher prevalence of psychiatric illness in people with DED compared to healthy controls (45.6% versus 12.8%, respectively). We chose to use the GHQ-12 as it is a well-known clinical instrument for measuring psychiatric disorders27 and is more specific to the needs of study.
In their 2016 study, Szakátset al. evaluated the correlation between Schirmer’s score and anxiety and depression indices (using Beck Anxiety Inventory [BAI] and Beck Depression Inventory, respectively); they found a significant inverse correlation between BAI and Schirmer’s scores.28 Tiskaoglu et al. also found results similar to the present study, with Schirmer’s test values being significantly lower in patients diagnosed with depression compared to patients without depression.29 However, Labbe et al., who also assessed a correlation of depression score with Schirmer test and TBUT, failed to derive a significant result.30 Li et al. also failed to find a significant correlation between depression scores and Schirmer’s and TBUT scores.31 Additionally, a study by Kim et al. did not yield a significant relationship between depression severity and Schirmer test.32 With regards to OSDI scores, Hallak et al. derived similar results to the present study, reporting significantly higher OSDI scores in patients with DED.26
One of the main reasons for the different picture in the present study with respect to the relationship between Schirmer’s test and incidence of psychiatric illness could be the difference in the method of assessment, as we did not conduct a linear correlation. Another reason could be that the age range of participants in the present study (20–40 years) differed from that of previous studies, which generally included elderly patients.33,34 Increased age could mean that psychiatric morbidity is confounded by factors other than DED. Thus, the present study could provide more useful information regarding the psychiatric impact of DED in a relatively younger population. Notwithstanding the difference in pattern and trend of psychiatric morbidities, almost all the previous studies have shown that patients with DED have an increased risk of psychiatric morbidity as compared to their matched controls.
Like other epidemiological studies, where females can account for up to two-thirds of the study population,2–6 females made up the majority of participants in the present study. In order to rule out the impact of age and gender, we purposely selected controls with matching age and gender.
Conclusion
The findings of present study provide useful information regarding psychiatric impact of DED in a relatively young population. This is the first study the authors are aware of to explore this relationship in an Indian population. This study, in general, supports the existing literature that a significant association between DED and psychiatric morbidity burden is present, while at the same time providing some newer information suggesting that the relationship between severity of DED and psychiatric comorbidity should not be viewed as a linear one and should be interpreted in context with the stage of disease, and more so in different life stages of the patient. To validate the findings of our study, further research is recommended in view of the fact that this is probably the first study in an Indian and relatively younger population.







