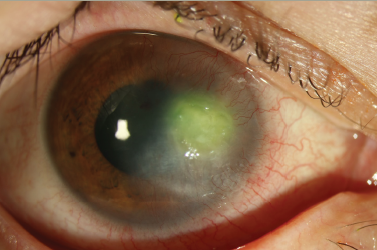
Q. Could you tell us a little about the microbubble technique in keratoplasty?
The microbubble incision technique is a new surgical method which exploits the presence of small air bubbles in the premembrane layers. This removes deep stroma to reach Descemet membrane by means of manual layer-by-layer dissection. This technique is particularly useful in case of failure to establish a normal big-bubble using the Anwar big-bubble method.1 We know that deep lamellar anterior keratoplasty (DALK) has strict indications, for example in keratoconus, and provides better long-term results than penetrating keratoplasty, not so much in terms of visual acuity but in terms of survival of the transplant and reduction of the risk of rejection. In light of this, all the techniques that facilitate a more rapid and effective DALK dissection, in case of failure of the conventional big-bubble, are welcome. In particular, several preliminary studies seem to indicate microbubble technique as an alternative promising option for the surgeon.2
Q. What are the limitations of this technique?
Further studies with large cohorts of patients and long follow up are needed to confirm first impressions about the microbubble incision technique because it remains a technique that is difficult to standardise and is strongly dependent on the surgeon.
Q. What are the advantages and limitations of corneal stromal demarcation line depth to assess collagen cross linking efficacy?
Corneal stromal demarcation line (DL) can be observed within the corneal stroma at 1 month post-operation. The interpretation of the depth of DL is certainly advantageous as it remains a reliable structural value and is now less operator-dependant thanks to the advent of recent optical coherence tomography devices which are able to easily detect the depth of DL. On the other hand, corneal stromal DL represents an indirect measurement of CXL penetration within the stroma. Current knowledge suggests that the ‘the deeper, the better’ principle is rather a simplistic approach for interpreting the clinical importance of the corneal stromal DL.3 However, we can be sure that DL remains one of the most reliable tools in evaluating efficacy of CXL treatment.
Q. What were the findings of your recent study comparing treatment protocols of corneal cross linking?
I have dedicated my efforts in cross-linking treatments since development of this technique began several years ago. Over the years, several changes have been made, improving the effectiveness, safety and comfort for the patient. Based on my experience and my studies about the latest CXL protocols I can attest that, within certain limits, the accelerated protocol after corneal disepithelialisation (Epi-off A-CXL) remains the most effective in stabilising ectasia in corneas thicker than 400 microns. The key word of the present and the near future regarding CXL is ‘customisation’, such that we utilise a protocol that is tailored to the patient where possible not excluding the association of CXL with corneal regularisation methods, the so-called ‘CXL plus’.
In thinner corneas, the safety parameters will guide us to one of the Epi-on treatments that can also be satisfactory in terms of effectiveness, although less so than the epi-off techniques.
Q. What presentations are you most looking forward to at this year’s European Society Of Cataract & Refractive Surgeons (ESCRS) meeting?
In the next ESCRS meeting I am mainly looking forward to the novelties about refractive surgeries. Moreover, I will be interested to hear about laser-assisted surgery and corneal lamellar transplants, which have now almost completely supplanted penetrating techniques. Finally, I will be especially focused on the relatively recent Descemet membrane endothelial keratoplasty technique and the innovations concerning the topic of endothelial keratoplasty.