Glaucoma is a chronic neurodegenerative disease characterised by retinal ganglion cell death. The loss of retinal ganglion cells results in typical structural changes in the optic nerve head (ONH) and the retinal nerve fibre layer (RNFL) and in distinctive visual field (VF) defects. Glaucoma is a leading cause of blindness in Europe, with a prevalence of 1–2% of the adult population. Most patients with glaucoma are undiagnosed due to its asymptomatic course.1
Glaucoma is a chronic neurodegenerative disease characterised by retinal ganglion cell death. The loss of retinal ganglion cells results in typical structural changes in the optic nerve head (ONH) and the retinal nerve fibre layer (RNFL) and in distinctive visual field (VF) defects. Glaucoma is a leading cause of blindness in Europe, with a prevalence of 1–2% of the adult population. Most patients with glaucoma are undiagnosed due to its asymptomatic course.1
Glaucoma diagnosis is based on the detection of the characteristic structural and/or functional changes and relies on the experience of the investigator. Most people diagnosed with glaucoma have corresponding structural and VF test abnormalities. However, in patients with early stages of the disease, the diagnosis may bechallenging as they may show only VF or structural changes.
The detection of VF defects often occurs after there has been substantial structural damage.2,3 Diagnosis of early glaucomatous optic nerve damage may be challenging even for experienced clinicians because of the wide variability of normal optic disc morphology. Sometimes the diagnosis of glaucoma in the absence of VF abnormalities is confirmed after monitoring patients and detecting structural changes in the optic nerve or RNFL.4
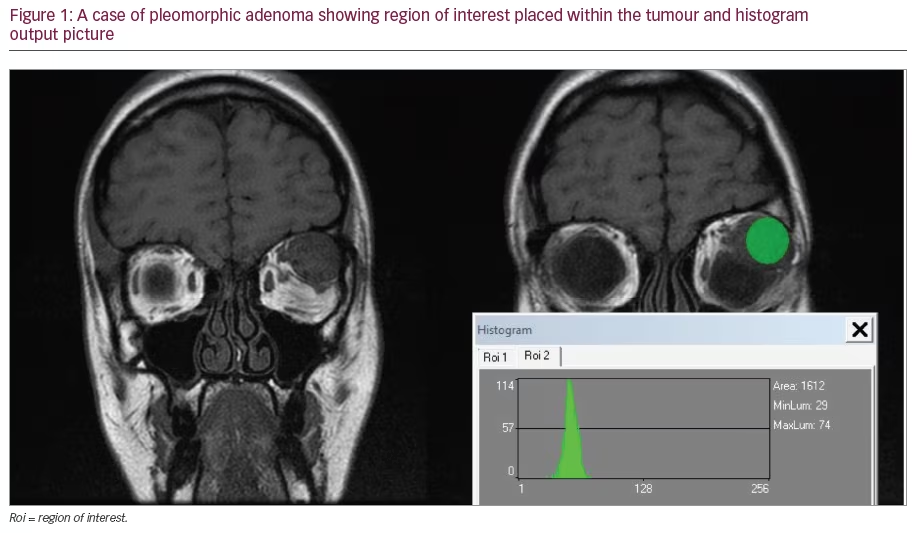
Until recently, the reference standard for recording ONH damage was stereophotography of the ONH and red-free pictures of the RNFL.5,6 Recently introduced imaging devices are designed to facilitate the objective and quantitative assessment of the ONH and the RNFL: scanning laser polarimetry (SLP, i.e. GDx), confocal scanning laser ophthalmoscopy (CSLO, i.e. Heidelberg retinal tomography [HRT]) and optical coherence tomography (OCT) (see Figure 1). They can be used to detect early structural damage by focusing on glaucoma-relevant structures of the ONH and surrounding tissues and using a normative database to determine the probability of glaucoma. Imaging of the ONH and the RNFL for detecting glaucoma progression is another important aspect of glaucoma management. However, in this review we will focus only on the role of imaging technologies in the diagnosis of glaucoma. We will provide a brief description of the recent advances, and review the current literature on the diagnostic performance for glaucoma of these imaging devices.
Scanning Laser Polarimetry
SLP is designed to provide objective assessment of the RNFL thickness with potential use for diagnosis and follow-up. SLP is based on the principle that polarised light passing through the birefringence RNFL undergoes a detectable phase shift, which is linearly related to RNFL thickness.7 The result is a 2D map of retardation around the optic disc. The software provides a discriminating classifier of glaucoma/normality named nerve fibre indicator (NFI), which is fully automated. To detect change over time, regression analysis can be performed.
The first GDx nerve fibre analyser contained a fixed compensating device to compensate for polarisation effects of cornea and lens. Because the parameters for corneal compensation are different for different eyes,8 the current SLP systems (GDx Variable Cornea Compensator [VCC] and GDx Enhanced Corneal Compensator [ECC],Carl Zeiss Meditec, Inc., Dublin, CA) include a variable compensator that allows for individualised eye-specific compensation of anterior segment birefringence. The performance of SLP can be affected by light scattering in the eye leading to a poor signal-to-noise ratio and atypical retardation patterns (ARPs).9–11 The reason for ARPs is unknown, but as ARPs occur more in glaucomatous eyes than in normal eyes it has been hypothesised that it results from low signalto- noise ratio when decreased reflectivity is present.9 An analysis of the contribution of backscattered light from various depths to the total retardation map using spectral-domain OCT found that atypical retardation patterns in SLT are associated with deep penetration of the probing light beam into the strongly birefringent sclera.12 To improve the accuracy, first the already-mentioned VCC,13 then the software-based ECC14 were introduced. It appears that GDx ECCperforms better than VCC in the detection of glaucoma in early stages of disease.11,15
Confocal Scanning Laser Ophthalmoscopy
Confocal scanning laser ophthalmoscopy (CSLO) is an imaging tool that is designed to create a quantitative, 3D topographic picture of the ONH and the posterior segment surface. The currently used instrument, the HRT (Heidelberg Engineering GmBH, Dossenheim, Germany), uses a 670nm diode laser beam to scan the surface of the posterior segment. Based on the measurements of the ONH, the instrument generates a number of stereometric parameters, such as rim volume, rim area, cup shape or cup-to-disc ratio, that allow evaluation of the ONH for glaucomatous damage. The relevant ONH parameters are automatically generated by the instrument’s software after identification of the optic disc border by the operator. It allows optic disc assessment to detect structural glaucomatous changes up to eight years earlier than visual field examination.16
The latest version of the CLSO, the HRT III, provides a large ethnicselectable normative database and includes data analysis tools such as Moorfields regression analysis (MRA) and the Glaucoma Probability Score (GPS). Other technical improvements in the scaling and alignment of images have been made.
MRA is a linear regression that takes into account the relationship between optic disc size and rim area or cup-to-disc ratio. The MRA improves the diagnostic accuracy of the HRT by taking into consideration that neuroretinal rim area is affected by disc size and age.17
The GPS is an automated approach to the optic disc classifying procedure that eliminates operator-dependent factors, which are a source of variability. It is based on five glaucoma-specific parameters of the 3D shape of the optic disc and peri-papillaryRNFL and provides disease probability values.18
The glaucomatous change can be assessed by topographic change analysis (TCA). TCA provides localised, objective and quantitative information about changes in the volume of the neuroretinal tissue. TCA describes significant repeatable changes in the neuroretinal rim volume by comparing the variability within a baseline examination with that between baseline examination and follow-up examination.19
Optical Coherence Tomography
OCT uses a scanning interferometer and a coherent infrared light (of 820–870nm) to obtain cross-sectional retinal images based on the reflectivity of the different retinal layers down to the retinal pigment epithelium.20 OCT is a non-invasive, cross-sectional imaging technique that allows in vivo measurements of tissue thickness. The most commonly used time-domain OCT device (Stratus TD-OCT model 3000, Carl Zeiss Meditec, Inc. Dublin) has an axial resolution of approximately 10 microns and a transversal resolution of approximately 20 microns.
With the OCT the topography of the ONH can be assessed; however, the most important aspect of the OCT is the quantification of the RNFL thickness, which is measured using peri-papillary scanning around the optic disc. Because the RNFL is one of the layers with the greatest reflectance and because of its anterior location, it can be automatically segmented and measured by computer algorithms.
There are major recent developments of OCT, such as spectraldomain optical coherence tomography (SD-OCT), which permits much faster scanning and better axial resolution than TD-OCT. 3D OCT is also available and may be used to image the ONH. There are several SD-OCT devices commercially available, and it is likely that further developments will appear in the future.
It is unclear whether the new SD-OCT technology will improve the diagnostic performance with glaucoma. It seems that this may be the case as a more accurate measurement technique for assessment of the thickness of the retinal layers is provided. The capability of the new SD-OCT to detect localised RNFL defects, documented on stereophotographs, was investigated. All currently available SD-OCT instruments were able to confirm the structural glaucomatous damage.21 It has been shown that RNFL thickness measurements obtained by SD-OCT correlated more strongly with localised visual field defects than scanning laser polarimetry.22
The relationship between RNFL thickness measured by timedomain (Stratus) and spectral-domain OCT (Cirrus HD; Carl Zeiss Meditec, Inc. Dublin) has been studied. A good correlation between the two instruments was found; however, when absolute values were compared, a significant difference in RNFL thickness was detected. Therefore, measurements are not interchangeable and cannot be compared directly. It was shown that RNFL measurements obtained by the Stratus OCT are generally higher than with the Cirrus OCT, except when the RNFL is very thin.23–25
Literature Review
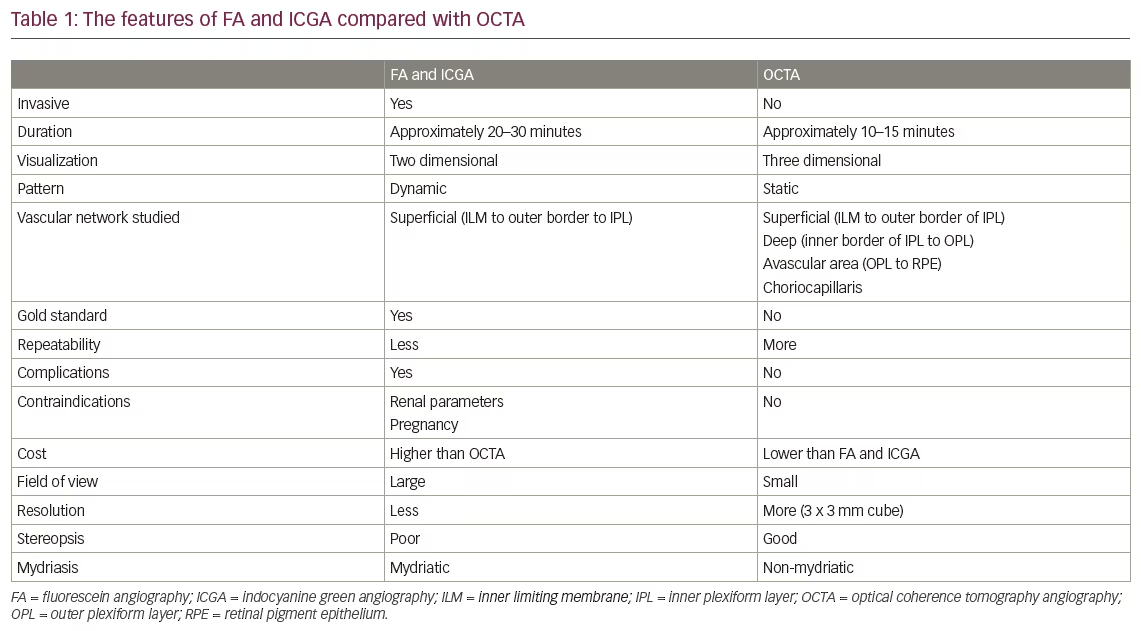
We have reviewed the most recent studies on diagnostic accuracy of the above imaging technologies, and assessed the quality of the studies. For this purpose we conducted a comprehensive search of peer-reviewed literature in PubMed for the period January 2007 to June 2009. The search was limited to studies published in English-language journals. The following search terms were used: optical coherence tomography, scanning laser polarimetry, confocal scanning laser ophthalmoscopy and glaucoma. The search resulted in 326 citations. The abstracts of these articles were reviewed, and 35 studies comparing different imaging instruments or reporting diagnostic performance of each of the three instruments were found. Only prospective studies were included (see Tables 1–3).
The quality of the selected articles was assessed using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool,26,27 a quality assessment tool using 14 items (see Table 4). As the interpretation of the test results using imaging devices for glaucoma is fully automated, the QUADAS tool was modified slightly and item 12 was removed. Among the QUADAS items, some appear to be of critical importance, e.g. ‘Was the spectrum of patients included in the study representative of the patients that will receivethe test in clinical practice?’ and ‘Was an appropriate reference standard chosen?’1,28
Asking if a population is representative is important to understand how the imaging devices perform in ‘real-life’ conditions, when patients with some media opacity, other ocular co-morbidities or poor co-operation are examined. Refractive error, disc size, severity of glaucoma or operator-dependent factors can also influence the performance of the imaging instruments. Including a large proportion of patients with more severe disease is associated with increased sensitivity.29
Regarding the performance of HRT in diagnosing glaucoma, the data analysis tools MRA and GPS were assessed. The ability of HRT to discriminate between early glaucoma and normality was similar to the assessment of stereoscopic disc photographs by expert clinicians.30 HRT could outperform stereophotography in one study, but the authors used non-mydriatic stereophotographs, which are not of optimum quality.31 The diagnostic performance of MRA compared with GPS was judged to be similar in some studies,32,33 while others reported a better performance of GPS34 or MRA.35
Regarding SLP (GDx), two high-quality studies were detected (i.e. using an acceptable reference standard, including a spectrum of disease and patients that is similar to the patients in whom the instrument will be used in practice). In these two studies, SLP was able to detect pre-perimetric glaucoma36,37 with reasonable accuracy. In other studies it was shown that ECC performed better than VCC.11,15
The performance of the different OCT instruments appears to be comparable.38,39 The Stratus OCT has a rather poor performance in preperimetric glaucoma.40,41 Differences in the RNFL configuration and thickness assessed by OCT were detected in eyes with OHT.42,43
Results of Studies Comparing Different Devices
The diagnostic performance of the different imaging devices is comparable and appears to be acceptable to diagnose glaucoma (see Table 5). However, there is very limited use in pre-perimetric glaucoma.44,45 The performance of the GDx VCC in a glaucoma screening trial was reported. A combination of several GDx parameters appeared to be useful for detecting glaucoma in the population,46 while the performance of HRT II was rated to be poor.
Frequency doubling technology (FDT) perimetry or stereoscopic disc examination by an experienced observer outperformed imaging devices in some studies.47,48 However, when less experienced graders assess the optic disc, imaging devices provide higher diagnostic accuracy.49
Among the most common limitations of the published literature, we would highlight that most studies compared eyes with already known and manifested glaucoma versus known healthy eyes. Four studies, two on OCT40,41 and two on GDx,36,37 investigated patients with preperimetric glaucoma. In only one study was the screening performance of an instrument (GDx) investigated.46 For detecting preperimetric glaucoma, the performance of OCT was poor.40,41 Both reports on GDx showed promise for detecting pre-perimetric glaucoma.36,37 It has to be mentioned that several studies examinedcommercially unavailable detection algorithms that may have a higher diagnostic accuracy than the standard diagnostic tools.
Both GPS and MRA easily detected glaucoma in large discs but performed worse in smaller discs. In general it was shown that GPS is influenced to a greater extent by the disc size and is therefore outperformed by MRA.50,51 It was suggested that GPS may be more useful to confirm a normal disc while MRA might be more helpful to confirm glaucoma suspects.52 SLP (GDx VCC and ECC) has been shown to be influenced only minimally by optic disc size; however, repeatability of the measurements decreased with increasingseverity of glaucoma.53
Conclusion
Recent advances in imaging devices for the assessment of optic disc morphology and RNFL thickness have the potential to greatly facilitate glaucoma diagnosis and monitoring of the disease. However, more high-quality studies on diagnostic accuracy are needed to define the role of imaging devices more precisely. At present is not clear which of the currently used imaging technologies is the most useful for diagnosis and management of glaucoma.