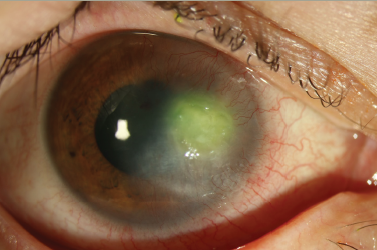
Trachoma is the leading infectious cause of blindness worldwide.1 Trichiasis, the end-stage of trachoma reflecting numerous episodes of infection with Chlamydia trachomatis, carries a high risk for subsequent visual loss due to distortion of the lid architecture and inturned eyelashes abrading the cornea. The World Health Organization (WHO) estimates there are 8.2 million people worldwide who suffer from trichiasis.2 The burden of trichiasis is likely even greater than would be measured by visual loss alone; one study found persons with trichiasis but no visual loss reported disruption of daily activities equivalent to that reported by persons with visual loss from other causes.3
Trichiasis Surgery
As part of a multifaceted approach to trachoma control, the WHO recommends surgery to correct trichiasis. Many techniques have been used to correct trichiasis, including epilation, cryoablation, tarsal advance and rotation, the Trabut method, Cuenod Nataf, and the bilamellar tarsal rotation procedure (BTRP). BTRP has been shown in a clinical trial to provide good long-term results compared with other techniques.4 In addition to improvement in ocular symptoms, trichiasis surgery appears to improve visual acuity, likely due to decrease in photophobia and resolution of corneal swelling.5 A handbook illustrating the correct techniques for BTRP has been published by the WHO.6 As trachoma is most endemic in resource-poor areas, it became immediately clear that there were insufficient ophthalmologists to reduce the backlog of trichiasis surgery, or handle new cases. Trichiasis surgeons were trained from the ranks of eye care nurses, medical assistants, and integrated eye care workers. A study of outcomes of trichiasis surgery, comparing ophthalmologists with these trained non-physicians, showed equivalent results, thus paving the way for surgery to be carried out at health posts, district centers, and even in the villages using this new cadre of manpower.7,8 The WHO has now published a manual for certification of trichiasis surgeons, which can be used by country programs to be certain that standards for undertaking trichiasis surgery are met.9
Adverse Outcomes of Surgery
However, some reports from trachoma programs based on outcomes after follow-up of trichiasis surgery patients paint a dismal picture. One study of trichiasis surgery cases with follow-up of at least two years, carried out in several districts of Tanzania, found a recurrence rate of trichiasis of 28%, varying by district from 16 to 38%.10 In The Gambia, trichiasis recurrence rates at one year were 41%, and varied among surgeons from 0% to >80%.5 Data from Oman also showed a high rate of recurrence, 56% on average three years post surgery.11 However, in controlled clinical trials under strict surgical conditions, adverse outcomes following surgery are low. In a clinical trial of BTRP, the adverse outcome rate (including recurrent trichiasis) at 18 months was 18%.4 In another large clinical trial using integrated eye care workers in Ethiopia, recurrence of trichiasis was only 10% at 12 months, and 30% lower if azithromycin was used post surgery.12 Clearly, the variable rate of adverse outcomes following trichiasis surgery suggests factors that could be altered to improve outcomes. Studies identifying such factors are crucial, as high rates of trichiasis recurrence following surgery undermine public confidence in trachoma control efforts and discourage patients from seeking surgery. The likelihood of trichiasis recurrence following surgery is a function of three main factors: characteristics of the surgical patient, surgeon skill, and the post-operative environment. Each factor is discussed in more detail below.
Characteristics of Trichiasis Surgery Patients
Once a patient has undergone trichiasis surgery, the risk for recurrence or lid-closure defects following subsequent surgeries is higher than the risk following initial surgery.4,13 Thus, from a program perspective it is even more critical to have low recurrence rates following the first surgery, as the risk for adverse outcomes following repair of recurrent trichiasis is so much greater.
Patients who present with more severe trichiasis, as quantified by increasing number of lashes touching the globe, or severe entropion are also at greater risk for recurrence. Patients with 10 or more lashes touching the globe were 70% more likely to suffer recurrent trichiasis at one year in a trial in The Gambia.5 In the Ethiopia trial, patients with the most severe entropion were three times more likely to suffer recurrence at one year compared with patients with mild entropion.12 Severe entropion at baseline was also a predictor of the severity of trichiasis recurrence at one year, with moderate to severe entropion associated with a 2.3–3.6 times increased risk for recurrence of five or more lashes touching the globe at one year.14 These findings argue for an earlier presentation of trichiasis for surgery, to ensure a more successful outcome. Patients who wait until the lid margin has been almost entirely inward deviated so that the lash base cannot be seen run a much higher risk for poor outcome of surgery. Other characteristics of patients have been studied in relation to recurrent trichiasis. Although females are at much higher risk than males of having trichiasis, they do not appear to be at any greater risk for recurrence once accounting for severity of trichiasis pre-operatively.5,13–15 A study in Oman found higher rates of recurrence in females compared with males—61% compared with 49% after a three- to five-year follow-up11— but did not control for level of severity at baseline. In settings where women may wait until trichiasis is quite advanced before seeking surgery, recurrence rates for them may well be higher and reflect gender rolemediated factors.16 Similarly, age alone does not appear to affect the recurrence rate of trichiasis following surgery.12,13,15,17 An increase in risk for recurrence with age of the patient disappears when adjusted for the confounding effects of severity of trichiasis prior to surgery.
Surgery Factors
It is clear that the skill of the surgeon is an important component of the outcome of the surgery. No other explanations can possibly account for the wide variation in recurrence rates between 0 and 80% in the study reported from The Gambia.5 West et al. found significant differences in recurrence rates between districts in Tanzania, where specific surgeons were assigned to a district and all were using the same surgical technique.15 An interesting report by Merbs et al. examined the pattern of recurrence to attempt to understand what components of the technique were problematic.18 They found a slight preponderance of recurrence for the left lid, and left side of the eyelid, suggesting a contribution of surgical technique to the recurrence of trachomatous trichiasis (TT). The authors concluded that, for right-handed surgeons, the awkwardness of maintaining a 3mm distance from the incision to the eye lid margin for the right side of the eyelid may lead to an incision that is inadvertently closer to the lid margin, with a resulting longer incision through the tarsus and potentially greater effectiveness of the rotation procedure. Ironically, an unintended modification of the standard BTRP procedure may have improved outcomes.
Surgeon factors can be ameliorated by proper training. In the Ethiopian clinical trial of antibiotic use in surgery, there was extensive use made of the certification of surgeons manual.9,12 There was no difference between surgeons in recurrence rate, which was very low. The trial found that use of azithromycin post surgery reduced recurrence by 30%, but the authors also speculated on two other factors that might have reduced recurrence rates overall: first, the surgeons were especially trained in sterile techniques and strict procedures for preserving a sterile field were in place during the trial. In our experience, that is one aspect that is overlooked in trichiasis surgeon training. Second, the sutures were left in place for two weeks rather than one week. The authors speculated that providing a longer period for maintaining the sutures would lead to a stronger adhesion between the surgical margins and more likely hold the lid margin correction. More effort to improve surgeon technique by country programs is needed. Ongoing surgical audit has been proposed, and the need to de-certify surgeons who perform below standard must be considered.19,20
A new trichiasis surgical tool has been developed with the goal of assisting the surgeon in proper placement of hemostats to avoid crushing the lid, and proper incision length and distance from the lid margin (Merbs, personal communication). Its impact on long-term outcomes of surgery is currently being evaluated in a clinical trial of trichiasis cases in Tanzania, among surgeons whose recurrence rates have been high.
The choice of technique also may affect the outcome. Bilamellar tarsal rotation was clearly shown to be superior to electrolysis and cryoablation, for minor trichiasis, and to tarsal advance and rotation for major trichiasis in terms of adverse outcomes.4 The one-year recurrence rate in Vietnam, using a modified Cuenod Nataf procedure, was 10.8%, which is similar to the one-year recurrence rate for the trial of BTRP.13 The patient populations were dissimilar, ophthalmologists performed the surgery in both studies, and severity of trichiasis at the outset was not graded in the Vietnam study, so it is hard to directly compare outcomes. There may also be an effect of suture material. An ongoing clinical trial is investigating the effect of absorbable versus non-absorbable sutures. With absorbable sutures, the loss to follow-up experienced by programs after surgery and granuloma formation around the retained sutures would be avoided.
As discussed below, recurrence rates appear to be higher if patients come from areas where active trachoma rates are highly endemic.11 The possibility has been raised that ongoing exposure to trachoma results in greater recurrence of trichiasis. Two clinical trials have now been completed to evaluate the effect of using a single dose of azithromycin immediately post-operatively to reduce recurrence. One trial showed no benefit, but the surgeons were not standardized and some had extremely high recurrence rates.5 It is not reasonable to expect added benefit from azithromycin where surgeon skill factors overwhelm the outcome. With greater numbers of cases and standardization of surgeons, the other trial showed no differences in outcome by surgeon and the recurrence rate was low.12 A single dose of azithromycin post-operatively reduced recurrence rates by 30% at one year compared with provision of topical tetracycline, which suggested added benefit in improved outcomes. However, there was no added benefit to treating the entire family of the case with azithromycin compared with treating the case alone.
Post-operative Environment
Trichiasis surgery cases come from villages where trachoma is endemic, or was formerly endemic. Persons with both scarring and infection with C. trachomatis were at greater risk for developing trichiasis than persons with scarring alone.21 Follow-up studies of surgical cases have found that post-surgical recurrence was highest in areas with the greatest trachoma prevalence.11,15 One study reported a higher rate of recurrence in surgical eyes with ocular C. trachomatis infection compared with eyes with no infection.22 However, the clinical trial in Ethiopia that found benefit in postoperative use of azithromycin could not attribute the protective effect to lower post-surgical rates of ocular C. trachomatis,12 with the caution that missed episodes of infection could have occurred between the data collection periods. While it is clear that risk for trichiasis is greatest for those living in trachoma hyper-endemic communities and at risk for multiple bouts of infection, it is not clear that recurrent trichiasis post surgery is due to ongoing bouts of C. trachomatis.
It may be that the wider systemic protection afforded by azithromycin’s broad spectrum of activity prevented other infections from contributing to recurrence. In a longitudinal study of trichiasis cases in The Gambia, bacterial infection at follow-up was associated with three-fold higher risk for recurrence.17 Of the operated eyes, 72% had samples taken, and 27% grew pathologic isolates, largely Streptococcus pneumonia and Staphylococcus aureus. The authors note that trichiatic eyes, with scarring replacing the normal conjunctiva, may be prone to bacterial conjunctivitis,which can lead to chronic inflammation and progressive cicatricial changes. It is also possible that the bacterial conjunctivitis was the result of recurrent trichiasis, rather than being a causal factor; the study’s crosssectional design did not permit analyses of the temporal relationship.
The home environment of these trichiasis cases in endemic villages is characterized by lack of water and difficulty in maintaining cleanliness. For patients with bilateral surgery, both of whose eyes may be bandaged postoperatively, the temptation to remove the bandages and expose the eye to such conditions may be irresistible. Early removal of bandages was postulated to be one reason why males were more likely to have recurrent trichiasis compared with females in Ethiopia.14
Conclusions
The World Health Assembly resolution WHA51.11 mandates that blinding trachoma be eliminated by 2020.23 Surgery to correct trichiasis is one of the pillars of the WHO Surgery, Antibiotics, Facial cleanliness, and Environmental Improvement (SAFE) strategy for trachoma control. High recurrence rates following surgery are destructive to national control programs because patients will, understandably, refuse surgery and eyes with recurrence are even more at risk for further recurrence following repeat surgery. With adequate training, standardization and certification, and supervision, trichiasis surgeons can achieve a low rate of recurrence. The addition of azithromycin post-operatively under these conditions can further reduce recurrence. Future research on devices to assist surgeons to achieve the best possible technique for surgery, and research on the role of sutures in preventing recurrence and other adverse events, will also ensure acceptable outcomes. Counseling patients to follow post-operative instructions on bandage removal and wound care must consider the local environment and the feasibility, and alternatives to, the recommendations.
Increasing emphasis on mass drug administration as part of emphasis on control of active trachoma appears to be diverting attention from the surgical needs of the group at highest risk for blindness from trachoma. Efforts to ensure the best outcome of trichiasis surgery for trachomaendemic, and formerly endemic, countries is imperative. Even with control of active trachoma, as achieved in Morocco, Oman, and now Ghana, trichiasis cases will continue to emerge from these communities for years. Detection of these cases, proper surgery and case management, is critical to achieving all the goals of the elimination of blinding trachoma.