This review of corneal wound healing following refractive surgery is modified and updated from a previous review of general corneal wound healing.1
To help understand the wound healing response after keratorefractive procedures, it is first important to review the structure of the cornea. Understanding the structure also can help explain some of the complications that can arise as a result of refractive surgery.
This review of corneal wound healing following refractive surgery is modified and updated from a previous review of general corneal wound healing.1
To help understand the wound healing response after keratorefractive procedures, it is first important to review the structure of the cornea. Understanding the structure also can help explain some of the complications that can arise as a result of refractive surgery.
Bowman’s layer is composed of 22nm heterotypical type I collagen fibrils, which are randomly orientated (mean direction 45º to the corneal surface).2 Immediately beneath Bowman’s membrane, the cornea is arranged such that there are about 300 lamellae centrally and 500 lamellae peripherally. Each is composed of uniformly paralleldirected, 25nm heterotypical type I collagen fibrils with flattened keratocytes present between some adjacent lamellae. In the anterior third of the stroma, lamellae are orientated in oblique directions to the corneal surface; they branch extensively and are interwoven with other lamellar layers both anteroposteriorly and horizontally.
The structure of the lamellae in the anterior third of the stroma most resembles the pericardium, which prevents overdilation of the heart and formation of aneurysms.3 However, the lamellar structure of the posterior two-thirds of the stroma most resembles that of the annulus fibrosis of the intervertebral disc, functioning to dampen the compressive forces placed on the disc without rigidly maintaining shape.4 The lamellae in the posterior stroma are orientated parallel to the corneal surface and are thicker and wider than anterior lamellae.
There have been reports of some anteroposterior lamellar branching in the mid-stroma and of frequent interfibrillar bridging filament networks composed of type VI collagen filaments present throughout the entire corneal stroma. Between the most posterior layer of the stroma and Descemet’s membrane is a thin 0.5µm layer of loosely arranged collagen fibrils and fibronectin. One explanation for the higher risk of ectasia after laser-assisted in situ keratomileusis (LASIK) compared with photorefractive keratectomy (PRK) therapy is that in LASIK the strongest portion of the cornea – the anterior stroma – in the thinner central (as opposed to thicker peripheral) cornea is transected for creation of the flap.
Basically, there are three histopathological types of wound healing after keratorefractive surgery,5 whether excimer laser ablation, penetrating keratoplasty6,7 or radial keratotomy:8–12
• hypercellular fibrotic stromal scar preceded by activated keratocytes;
• epithelial hyperplasia or hypertrophy; and
• hypocellular primitive stromal scar.
All of these can be identified with light, electron and immunofluorescence microscopy (or, with less detail, by confocal microscopy).12
In animals, it has been demonstrated by in vivo confocal microscopy and immunohistology that there are three morphologically and functionally distinct types of keratocyte. These arise from the normal, quiescent, undamaged keratocyte population after corneal stromal injury, whether mechanical, chemical or by excimer laser:
• a migratory keratocyte (which mobilises and repopulates acellular regions);
• an activated keratocyte (which synthesises, deposits and degrades the extracellular matrix); and
• the myofibroblast (which initiates wound contraction).13,14
In LASIK, keratocytes undergo apoptosis in a zone 50µm anterior and 50µm posterior to the central and paracentral lamellar incision over the first 24 hours after surgery.15–18 Keratocyte proliferation starts four hours after injury and ends about one week after injury. Following this, minor apoptosis continues and minor keratocyte necrosis occurs from 24 hours to one week; inflammatory cell infiltration occurs from four hours to one week; keratocyte cell migration occurs at three daysto three weeks from the periphery; and keratocyte differentiation occurs one to six weeks in the central flap and from one week to potentially more than three months at the flap margin.15–20
Keratocyte differentiation, whereby the altered keratocytes can appear and/or persist (as activated keratocytes and as myofibroblasts), is a determining factor in clinical haze noted by the examiner (although not necessarily by the patient).14 Myofibroblasts scatter significantly more light than normal quiescent keratocytes do. Conversely, although a cornea may appear clear by clinical examination, these altered keratocytes may give rise to complaints about visual quality – reduced contrast sensitivity, glare dysfunction, even reduction in bestcorrected visual acuity.21 Luckily, for most LASIK patients this hypercellular reaction occurs at the flap margin.
Some of the activated keratocytes become myofibroblasts and along with corneal fibroblasts participate in stromal remodelling through the production and reabsorption of collagen and production of glycosaminoglycans. It is interesting to note that these basic patterns of wound healing are consistent across different types of corneal injury and/or surgery. For example, activated keratocytes are found in human corneas implanted with intrastromal corneal ring segments and removed for penetrating keratoplasty.22
The provisional corneal wound matrix, which is rich in fibronectin and chondroitin sulphate, promotes the entry of migrating fibroblasts into the wound area.1,23 Expression of alpha-smooth-muscle actin, a smooth-muscle-specific protein, has been used as a chemical marker for myofibroblast transformation. In incisional wound healing, it is known that adjacent keratocytes transform into a smooth-muscle-like myofibroblast phenotype in response to corneal injury.14,24 A major
mediator that triggers keratocytes to become myofibroblasts is transforming growth factor-ß2.24
In a post mortem study of post-operative (two months to 6.5 years) human LASIK corneal wounds, it was found that a stromal interface scar of variable thickness is produced during the time of active corneal wound healing. The epithelium displays focal, outward compensatory hyperplasia at the flap margin.13 Causing a lesser degree of epithelial thickening, there are focal areas of inward basal epithelial cell hypertrophy into the valleys produced by underlying microstriae in the LASIK flap. In short, the thickened epithelium in successful LASIK is due to inward elongation of basal epithelial cells, thickening, wrinkling and reduplication of the epithelial basement membrane and undulations of Bowman’s layer.25 Overall, there was a 1.3–3.2µm increase in the average thickness of the central corneal epithelium in post mortem corneas compared with normal control corneas.13 This study found no evidence of outward epithelial hyperplasia over the flap except at the wound margin.
The epithelial changes documented by Artemis very-high-frequency digital ultrasound arc scanning technology (ArcSan, Inc.) may be enough to mask ectatic stromal changes (e.g. forme fruste or frank keratoconus), a contraindication for laser refractive surgery, primary or enhancement.26
In the study of post mortem post-LASIK corneas mentioned above,13 the LASIK flap wound, whether created by a microkeratome or laser, is described as consisting of two distinct types and regions of healing. The first type is a fibrotic, hypercellular scar at the flap margin, which is usually clinically visible and functions to hold the flap in place. The second healing type is a central hypocellular primitive scar that is not as visible and lacks collagen fibrils (the insoluble connective tissue component important for tensile strength). Instead, it has abnormally arge, non-fibril-bound proteoglycans.13,27 It is described as fibrotic because it is predominantly composed of a dense network of normal diameter (approximately 26nm) collagen fibrils and by immunofluorescence the scar contains more collagen type 3 than the normal corneal stroma. It also has similar levels of collagen types 1, 5 and 6, dermatan sulphate and keratin sulphate.13
By contrast, the extracellular matrix of the scar in the paracentral and central portions of the LASIK wound is described as primitive because it is primarily composed of electron-dense granular material with only loosely scattered, smaller-than-normal-diameter collagen fibrils (approximately 21nm). Based on immunofluorescence, the scar contains amounts of collagen type 1 similar to normal corneas, slightly less collagen type 6 and keratin sulphate, and markedly decreased collagen type 5. The scar has no detectable amounts of collagen type 3 and dermatan sulphate compared with those of normal corneal stroma.13
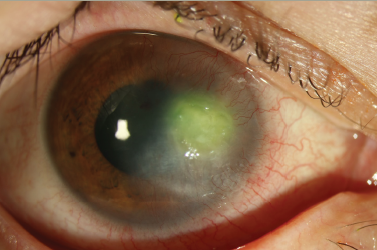
This hypocellular area does not undergo remodelling and is permanently weak in cohesive tensile wound strength (radial stress–strain behaviour). It is such that in post mortem post-LASIK corneas, the cohesive tensile strength of the hypocellular scar was described as 2–3% (0.75g/mm) of the normal corneal tensile strength (30g/mm).2 As a potential space, this hypocellular region is the reason for the risk of flap dislocations even a decade after LASIK. It is also the reason for interface complications, such as epithelial ingrowth, interface fluid syndrome, diffuse lamellar keratitis, interface fluid syndrome and infection.2 By contrast, the hypercellular area at the LASIK flap margin undergoes remodelling up to 3.5 years after surgery. In post mortem post-LASIK corneas it has a mean cohesive tensile strength that is 28% of the normal value, even almost 10 years after surgery.2
A longitudinal study was carried out on stromal keratocyte density (the subepithelial hyper-reflective stroma scar and the anterior unablated stroma) using confocal microscopy up to five years after PRK and LASIK surgery. There was a loss of the anterior 10% stromal keratocyte population after PRK, presumably from keratocyte apoptosis and necrosis.28 The anterior stroma was acellular for the first few days after PRK, but after a few months there were more keratocytes compared with the pre-operative ablated stroma. Thereafter, cell loss averaged 3.2% per year up to five years after surgery, such that at five years there was a 19.4% deficit relative to the pre-operative unablated stroma. Neither this study nor another longitudinal study found a marked change in cell density of the mid-stroma or posterior stroma.29
Regarding the status of endothelial cells after LASIK, in a five-year outcome study there was a statistically significant decrease in endothelial cell density – 1.2% over five years – which is likely to be within the range of physiological, age-related loss.30 However, there is documentation of endothelial cell loss one and three months after PRK with 0.02% concentration applied for 30 seconds.31
Matrix metalloproteinases (MMPs), of which there are at least 20 types in humans, are a family of proteolytic enzymes that are the principal mediators of tissue remodelling in physiology and pathology. They have been found in corneas following major and minor LASIK complications. MMPs degrade components of the extracellular matrix and basement membrane. In order to avoid uncontrolled and excessive tissue destruction, their expression is tightly regulated; they are typically secreted in a latent form that undergoes internal cleavage to be activated. They may perform a surveillance role in the normal cornea, catalysing degradation of collagen molecules that occasionally become damaged.1
In a study of LASIK corneas with minor flap complications, MMPs when present were localised exclusively at the flap margin and their presence was correlated with specific histopathological findings at the wound margin.32 MMP-9, a gelatinase, stained most strongly in the largest number of corneas. Experimental models have demonstrated a causal relationship between overexpression of MMP-9 in the corneal epithelium leading to basement membrane dissolution and/or failure to heal.33,34 The presence of MMP-9 in association with a disrupted basement membrane around an area of epithelia ingrowth suggests chronic, ongoing tissue remodelling. This might explain the finding that the weakest wound margin scars are those associated with epithelial ingrowth.27
Conclusion
In conclusion, corneal wound healing following laser refractive surgery follows a pattern of:
• epithelial changes (mostly hypertrophy);
• keratocyte apoptosis, activation and differentiation into myofibroblasts;
• recruitment of fibroblasts;
• absorption, remodelling and deposition of a new extracellular matrix; and
• formation of both hypercellular and hypocellular stromal scarring.
The same elements of wound healing follow other types of corneal surgery (intrastromal corneal ring segments) as well as trauma. Elucidation of the signalling components remains an important area of research. It is remarkable that despite biological variability in the millions of individuals worldwide who have undergone LASIK or PRK surgery, the pattern of wound healing is conserved andkeratorefractive surgery enjoys excellent results in general.