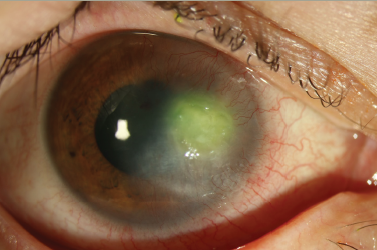
Corneal endothelial failure is a common cause of corneal transplants. According to the Eye Bank Association of America, transplant tissue distributed for endothelial keratoplasty accounted for 18,221 (43%) of all keratoplasties performed in the US during 2009.1 Fuchs dystrophy, other causes, and post-cataract surgery edema were identified as the leading indications for endothelial replacement surgery.
The main indicator, Fuchs endothelial dystrophy, is an inheritable genetic condition that results in loss of endothelial cells and formation of an abnormal extracellular matrix. It affects 5% of persons over 40 years of age2 and occurs three times more frequently in women than in men.3
Beginning in 2005, selective endothelial replacement gained momentum as the treatment of choice for endothelial pathologies. While a successful surgery, penetrating keratoplasty for primarily endothelial failure removes a significant amount of otherwise normal corneal tissue. Risk factors, including challenging intraoperative events, can complicate penetrating keratoplasties and unpredictable post-operative astigmatism may compromise outcomes and patient satisfaction.Finally, allogenic graft rejection is more common in penetrating than endothelial keratoplasties.4
Allograft Insertion
Endothelial keratoplasty is the targeted removal of pathologic host endothelium and Descemet membrane and replacement with a donor allograft consisting of a stroma–Descemet–endothelium complex created manually or using microkeratome dissection. The donor posterior ‘button’ is trephined in the operating room to fit the recipient bed, which is most often 7.5–9mm in diameter. The thickness of the donor allograft varies, and one study has demonstrated better post-operative visual acuity when tissue thickness is ≤131μm.5 After the donor posterior lamella is coated with a small amount of cohesive ophthalmic viscoelastic, it is separated from the anterior cap, 60–40 folded, and inserted with forceps into the anterior chamber. The forceps are opened and gently removed from the anterior chamber, carefully avoiding damage to the graft endothelium or changing its stroma-to-stroma orientation. Once the graft is unfolded andpositioned near the posterior stroma, an air bubble is injected to affix the donor tissue to the host. After a short time, the bubble is partially drained and the patient is assessed for adequate graft attachment. In most cases, the graft adheres to the host and the remaining air bubble resorbs in a few days. The pump action of the healthy donor endothelium begins to restore corneal transparency. The critical techniques are inserting the donor button while maintaining endothelial integrity, controlling graft position, and central deployment.
Incumbent Donor Insertion Techniques
There are various techniques for inserting the donor endothelium, which can be categorized into forceps, pull-through, and custom-deviceassisted delivery methods. Single-point fixation forceps attempt to minimize creasing and compression force along the length of the blades.When the forceps are closed the tips coapt, and the blades remain slightly separated while securing the folded tissue. Forceps insertion does not protect tissue from compressing during passage through the incision. Pull-through techniques use a guide that holds folded or unfolded tissue, depending on which device is used. Trephined donor tissue is loaded on the guide and placed at the incision to hold it agape. Through a second incision, opposite from the first, specialized long-arm forceps are inserted across the anterior chamber and used to pull the graft into position. In many instances, donor tissue is passed through a 5mm incision, which has been shown to cause less post-operative endothelial cell loss than smaller wounds. Forceps and pull-through guides can be used with incisions sized approximately from 3.0 to 5mm. While smaller incisions provide more anterior chamber stability, less iris prolapse, and less astigmatism than 5mm incisions, they result in significant donor endothelial damage. A vital dye study reported by Terry et al.6 demonstrated that smaller incision size contributed to decreased endothelial cell density when using either forceps or pull-through techniques. These techniques, while technically challenging, have contributed to the successful advancement of endothelial keratoplasty.
EndoSaver™
The EndoSaver is a unique single-use, disposable device used to efficiently and precisely implant donor allograft tissue during endothelial keratoplasty (see Figure 1). It is designed to carry graft tissue that is ≤175μm thick and 8.5mm or less in diameter. The patented tissue loading and deployment system gently retracts the graft with minimal manipulation into the insertion sheath (see Figure 2), then deploys it through a 4mm incision without plunging, pulling, or folding. Tissue is deployed in the anterior chamber by putting the tip of the insertion sheath at the far edge of the recipient bed, then moving the EndoSaver finger control to uncover the graft (see Figure 3). As the graft is gently deployed, the surgeon can control its precise placement without any instrument interference. Accurate placement occurs as the insertion sheath withdraws back through the incision, centering the graft in the bed. The luer connection allows irrigation through the device to control chamber depth. Due to the variations in regulatory clearance processes, outside the US the device is sold as EndoSaver. In the US, it will be sold as EndoSerter™. No differences exist other than the name.
In two North Carolina institutional review board (IRB) studies, the EndoSaver has been used to successfully implant more than 250 endothelial allografts. Study surgeons have found that the device’s intuitive design deploys the allograft accurately, requires no additional tissue manipulation, and simplifies and shortens the procedure. The authors describe their experiences using the EndoSaver when performing endothelial keratoplasty, and report six-month endothelial cell counts.
Methods
We enrolled 318 patients with endothelial cell failure in a prospective, interventional, non-randomized, uncontrolled trial as per an IRBapproved protocol. Patients with glaucoma, macular edema, macular ischemia, trauma, corneal scarring, artery occlusions, and vitreous hemorrhage were not included in the study. Patients with previous corneal transplants were excluded from the study as well. Detailed ophthalmic examinations were performed pre- and post-operatively, including best corrected Snellen visual acuity, biomicroscopic evaluation of the anterior segment, and dilate fundus examination with a 90D lens. This resulted in 43 patients being excluded from the study. 131 patients did not have follow-up adequate to complete their statistical analysis at the time of this publication. Thus, data were analyzed for 144 of the remaining patients who underwent EndoSaver endothelial keratoplasty.
Results
Surgery for 52 patients was performed by surgeon 1, and for 92 patients by surgeon 2. The patient sample consisted of 66.3% women. The mean age was 72 years (range 42–86). Ninety-seven patients had Fuchs dystrophy and 21 patients had pseudophakic bullous keratopathy. The mean air tampanade time was 9.27 minutes. Between the two surgeons, the mean six-month endothelial cell loss was 29.9%. The mean loss for surgeon 1 was 29.5% and for surgeon 2 was 29.9%. The average graft thickness was 102 microns. The mean endothelial cell loss at six months was calculated relative to baseline cell density provided by the eye bank. All donor tissue was pre-cut. Donor endothelial density was not re-evaluated immediately before surgery, therefore no recalculation of cell density was made secondary to variation between eye bank readers, differing post mortem preservation times, loss of epithelium, or Descemet folding. The mean endothelial cell loss at six months according to graft thickness is shown in Table 1. Seventy-one patients (49%) had 20/40 or better vision at six months. Ninety-five patients (66%) had 20/60 or better visual acuity. Five (3%) patients had a visual acuity of 20/70 or worse.
Discussion
With the growing number of advanced techniques and improvements in visual outcome, endothelial keratoplasty has become the standard of care for the surgical treatment of corneal endothelial pathology. Our study indicated that the EndoSaver is the superior option when compared with the forceps insertion technique for endothelial keratoplasty. The data indicate that between two surgeons and centers there is little variability in final endothelial cell counts at six months. Visual outcomes were also comparable to those in other reports.5
The EndoSaver is the only instrument capable of small-incision clear cornea surgery that requires no additional instrumentation. The advantages of topical EndoSaver endothelial keratoplasty include a smaller incision and no needle for retrobulbar block, thereby eliminating the risk of hemorrhage or globe perforation. Efficiency and cost savings are accomplished because there is no need for sutures, conjunctival incision, or cautery. Accordingly, EndoSaver use during endothelial keratoplasty results in reduced surgical risks and decreased operating room costs. We calculate that the price of EndoSaver is easily offset by elimination of these materials and their approximate cost: sutures ($30); disposable cautery ($20); anterior chamber maintainer ($32); and reduced operating room time ($200): total: $282. In addition, if the descemetorhexis is accomplished under air, the cost of a viscoelastic ($175) and irrigation– aspiration cannula (such as Simcoe, $40) can be added to the savings. EndoSaver use results in total savings of approximately $500 compared with the costs of forceps insertion. The authors have been impressed by the device’s ability to simplify the surgical procedure, accurately deliver and place tissue through a small wound, and its integral irrigation to maintain a deep chamber. A comparison of EndoSaver with other techniques is presented in Table 2.