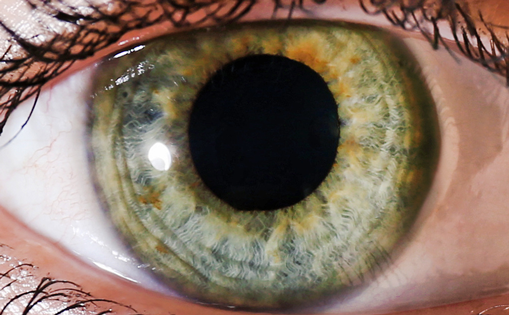
Pseudoexfoliation syndrome (PEX) is a common condition that may represent a serious challenge during cataract surgery.1 Prevalence in the US is up to 14% and is related to aging and low climatic temperature.2 Also known as ‘Viking disease’, PEX is more common in Northern Europeans: in Sweden, an 87-year-old individual has a 61% chance of having PEX.3 Pathological features include deposition of a white fibrillar material in the anterior segment of the eye, and this matrix of granular amyloid-like proteins can be found also in other organs.1
Postoperative inflammation is higher in PEX versus routine cataracts.1 This is due to a constitutively damaged blood-ocular barrier that leads to increased leakage of serum proteins into the aqueous humor after surgery (flare or Tyndall effect). The fragility of the blood-ocular barrier and intense postoperative inflammation may be responsible for a higher risk of pseudophakic macular edema in PEX eyes.1
Ophthalmic non-steroidal anti-inflammatory drugs (NSAIDs) are approved for the treatment of inflammation and pain after cataract surgery.4 NSAIDs have also been shown to prevent formation of postoperative macular edema in some studies.5 Nevertheless, it is debated if topical NSAIDs may be as effective as steroids in controlling inflammation after cataract surgery and there is lack of consensus about whether they should be given on routine basis in addition to topical steroids.6
A recent clinical trial demonstrated that bromfenac ophthalmic solution significantly reduced inflammation after cataract surgery when added to dexamethasone eye drops in patients with PEX.7 Sixty-two patients with cataract and clinical signs of PEX were randomized to dexamethasone 0.1%/tobramycin 0.3% ophthalmic solution alone (Group 1) or with the adjunct of bromfenac ophthalmic solution 0.09% (Group 2). All patients were examined on the day of surgery (baseline) and at postoperative days 1, 3, 7, and 30. Laser flare photometry was used to precisely quantify anterior chamber inflammation and optical coherence tomography (OCT) to measure macular thickness. Flare was 31% lower in Group 2 versus Group 1 at postoperative day 3 (11.92±8.14 versus 17.13±9.03 ph/msec; p=0.025) and 43% lower at day 7 (10.77±6.17 versu 18.72±12.37 ph/msec; p=0.003). There were no significant differences between groups in postoperative visual acuity, symptoms and ocular pain. Mean macular thickness at 1 month post-surgery was increased in Group 1, but not in bromfenac recipients (261.10±34.50 versus 243.38±28.23 microns; p=0.03). The incidence of intraretinal cysts at OCT was higher in Group 1 (n=4) versus the bromfenac group (n=0).
Pseudophakic macular edema is due to the breakdown of the blood-retina barrier.8 Eyes with PEX are at higher risk of developing pseudophakic macular edema.1 The incidence and the effects of subclinical macular edema after phacoemulsification on vision are probably underestimated.8 The current study showed increased macular thickness at postoperative week 4 in patients not treated with bromfenac. Although the study was not designed to adequately estimate macular edema, the difference in central macular thickness at OCT between the two groups was statistically significant. This difference could be clinically relevant because changes in macular thickness as low as 10 microns may have a considerable effect on contrast sensitivity. Interestingly, intraretinal cysts on OCT were not detected in any bromfenac recipients, but four patients receiving standard care developed subclinical cystoid macular edema at week 4.
Use of laser flare photometry in this study made it possible to accurately measure anterior chamber inflammation. This method is objective and highly reproducible.9 Most published studies on topical NSAIDs after cataract surgery were based on subjective slit lamp evaluation of postoperative inflammation by an ophthalmologist. These grading systems were based on uveitis studies and might be inappropriate to evaluate clinical conditions where the amount of postoperative inflammation is minimal, such as after uneventful phacoemulsification. The updated Laser Flare Meter FM-700 (Kowa Company, Ltd., Aichi, Japan) can precisely differentiate anterior chamber flare on a scale from 2 to 1000 ph/msec.
This study analyzed the effect of steroids and NSAIDs in a specific population (i.e., patients with PEX) and found that the combination of the two provided better anti-inflammatory effects than topical steroids alone. Laser flare meter and high-resolution OCT should be used in larger populations in order to study the effects of topical steroids and NSAIDs, alone or in combination, on intraocular inflammation after cataract surgery.