Epithelial basement membrane dystrophy (EBMD) and Fuchs endothelial dystrophy are two of the more commonly encountered corneal conditions in comprehensive and anterior segment ophthalmology practice. In many cases, epithelial basement membrane abnormalities, in the presence of endothelial disease, can be attributed to primary endothelial failure leading to corneal oedema and subsequent epitheliopathy. This article will provide an overview of both EBMD and Fuchs endothelial dystrophy and will discuss the role of epithelial debridement for epithelial basement membrane abnormalities in the setting of endothelial disease. We will also present a long-term update of our post-treatment results from patients in a previous report1 and also present two more cases of epithelial debridement performed after endothelial keratoplasty.
Epithelial Basement Membrane Dystrophy
Since its initial description by Cogan in 1964,2 EBMD has been recognised as the most common corneal epithelial dystrophy, affecting up to 76% of adults over 50 years of age.3 Also called mapdot- fingerprint dystrophy and Cogan’s microcystic dystrophy, the characteristic slit-lamp findings in EBMD result from re-duplication of the epithelial basement membrane.2,4,5 Surface epithelial irregularity can cause irregular astigmatism, glare, monocular diplopia, overall reduction in visual acuity and recurrent erosion syndrome. Medical treatment of the symptoms includes topical lubrication, hypertonic saline eye drops, soft and hard contact lenses and cycloplaegia. The two main indications for surgical treatment in EBMD are decreased visual acuity and symptoms of recurrent corneal erosions. Epithelial debridement, with or without diamond burr polishing of Bowman layer, is a safe and effective procedure preferred by many corneal specialists for its excellent results and its ease of performance at the slit-lamp or in the minor procedure room.6–14 The purpose is to mechanically remove the re-duplicated basement membrane and devitalised epithelium so that new epithelium may migrate in and form a smoother surface.
Gentle polishing of the Bowman layer with diamond-dusted burr may have the added theoretical advantage of removing more defective epithelial basement membrane and of promoting stronger adherence of the new epithelium. Aggressive debridement is not recommended: recent evidence from in vivo confocal microscopy suggests that the presence of a partially intact Bowman layer may possibly facilitate earlier recovery of corneal transparency and epithelial innervation.15 Itty and associates have reported the largest retrospective case review to date of simple mechanical epithelial debridement for treatment of EBMD, with 74 eyes of 55 patients.7 Eighty-two per cent of patients reported visual symptoms prior to epithelial debridement. Visual acuity improved from a mean of 20/44 pre-operatively to a mean of 20/33 postoperatively with a mean follow-up of 33 months. Recurrence of disease was noted in 24%, but only two patients required repeat debridement. The mean refractive change was -0.6D (range -4.75 to +2.0D). Similar results using debridement with polishing were noted by Tzelikis and associates with a mean follow-up of 22 months.12 Another study using diamond burr polishing for visually significant EBMD also did not observe any recurrences, although the mean follow-up was only 10.6 months.8
In a prospective, double-masked, randomised, controlled trial, Wong and colleagues investigated debridement techniques in 48 patients with recurrent erosion syndrome secondary to EBMD or trauma.13 Patients received either simple epithelial debridement with cellulose sponge or epithelial debridement with diamond burr polishing and superficial keratectomy. Major recurrence defined as epithelial defects occurred in 56.5% of patients in the epithelial debridement group and 4.0% of patients in the diamond burr group. Minor recurrences (defined as pain, redness, tearing and photophobia not severe enough for the patient to seek medical care) occurred in 65.2% in the epithelial debridement group and 20.0% in the diamond burr group. In retrospective case studies involving multiple surgeons and a varied number of cases, the difference between the two groups is less pronounced, with recurrence of recurrent erosions occurring in 11–18% in patients undergoing simple debridement7,9 compared with 4–25% in patients undergoing debridement combined with diamond burr polishing.6,9–11
Aldave and colleagues recently reported on the largest series of debridement with polishing by a single surgeon for visually significant EBMD and recurrent erosions.6 With a mean of 14.2 months of followup, there were no recurrences of dystrophic changes. Given these results and those in the literature, Aldave suggested there is a potential benefit to polishing the Bowman layer in all patients with EBMD to prevent recurrence of dystrophic changes.6 Other surgical options for treating symptomatic EBMD include anterior stromal micropuncture by needle16,17 or neodynium:yttrium– aluminium–garnet (Nd:YAG) laser,18,19 and excimer laser phototherapeutic keratectomy.11,15,20
Epithelial Basement Membrane Abnormalities in the Setting of Endothelial Dysfunction
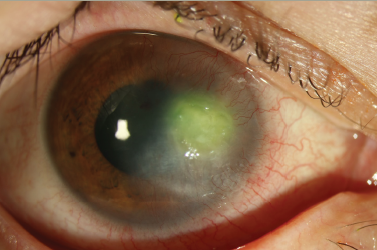
Findings similar to EBMD have been associated with chronic corneal oedema attributable to endothelial disorders. Clinically, it has been observed in Fuchs endothelial dystrophy, for example.21–24 Accordingly, histopathological characteristics of EBMD have been noted in 55.6% of eyes with chronic corneal oedema.22 Features described included typical EBMD with findings such as corneal epithelial reduplication, ectopic intra-epithelial deposits of basement membrane material and devitalised cells trapped in intra-epithelial pseudocystic spaces.22 Such changes were noted in 62.8% of eyes with Fuchs endothelial dystrophy and in 48.9% of eyes with pseudophakic bullous keratopathy or aphakic bullous keratopathy,22 two other important causes of endothelial failure. EBMD has also been reported in iridocorneal endothelial syndrome (ICE),25 a condition of unknown aetiology in which abnormal endothelial cells gain characteristics of epithelial cells.
Addressing significant EBMD prior to treatment of the underlying endothelial pathology can delay the need for more definitive therapy of endothelial diseases such as Descemet stripping automated endothelial keratoplasy (DSAEK). It may also help prepare the eye for more predictable cataract surgical outcome by enabling more accurate measurement of keratometry and calculation of intraocular lens implants.14 We previously reported on using epithelial debridement, a widely accepted method of treating EBMD, to treat the epithelial changes coincident with endothelial disorders.1 We herein describe our results and provide longer follow-up of the case series, illustrating different clinical scenarios in which epithelial basement membrane debridement was useful in patients who had EBMD associated with endothelial disease (see Table 1).
Patient 1, with Fuchs endothelial dystrophy, had debridement in one eye, which allowed for reliable biometric calculations for phacoemulsification and intraocular lens implantation (phaco/IOL). Debridement was performed for the contralateral eye 17 months after the initial phaco/IOL. At her post-treatment two-week follow-up, best spectacle-corrected visual acuity (BSCVA) was 20/70 with smooth epithelium, limited by 1–2+ stromal oedema. Subsequently, the patient was lost to follow-up and expired from metastatic bladder cancer several months later.
Patient 2, originally referred for combined phaco/IOL and penetrating keratoplasty for iridocorneal endothelial syndrome (ICE) of the right eye, experienced significant improvement of keratometry and topography readings after epithelial debridement. She was then able to undergo phaco/IOL alone, which improved vision to 20/25+2. Three months after cataract extraction, the patient developed stromal oedema and BSCVA was reduced to 20/50-2. DSAEK was performed at this point and final vision was 20/25-1 at two years after DSAEK with manifest refraction of -0.25+0.50×45.
Patient 3, with Fuchs endothelial dystrophy, underwent bilateral debridement. The right eye then underwent DSAEK, which was complicated by cystoid macular oedema, graft dislocation and ultimate graft failure. Subsequently, penetrating keratoplasty was performed and final BSCVA improved to 20/50-2.
Overall, the mean change in BSCVA post-operatively was two lines improvement in Snellen acuity (range zero to three lines) at onemonth follow-up. All of the eyes showed significant keratometric and topographic normalisation. Furthermore, epithelial debridement was refractively neutral, unlike in the study by Itty and associates,7 which showed a wide range of refractive changes. Three of our five eyes experienced a decrease in pachymetry values post-operatively, including one eye with ICE syndrome that had over 100μm decrease in total corneal thickness after simple epithelial debridement. In one report of patients with Fuchs, with and without epithelial oedema, the average difference in pachymetry was 58μm.26
Although epithelial debridement of EBMD in the setting of endothelial disease may be temporising, it is nonetheless a useful measure to improve ultimate visual outcome. In our series, the need for definitive keratoplasty in two eyes was delayed for three and five months, at which time DSAEKs were successfully performed. One case (patient 2) for whom penetrating keratoplasty was initially planned was able to receive DSAEK because of significant normalisation of the epithelium after debridement. In other cases, debridement allowed for reliable biometric calculations for cataract extraction and delay of DSAEK, with ultimate significant improvement in visual acuity.
Here, we also present two patients in whom epithelial debridement for EBMD after DSAEK lead to favourable visual outcomes.
In case 1, an 85-year-old female underwent uncomplicated cataract extraction in the left eye. Non-visually significant EBMD was noted bilaterally at the time of cataract surgery. Four years later, she developed pseudophakic bullous keratopathy in the left eye and experienced progressive decrease in vision. She received DSAEK in the left eye for visual rehabilitation. One month after DSAEK, the patient complained of irritation and foreign body sensation. Significant (3+) EBMD changes with epithelial bullae were noted. Intraocular pressures were normal. The DSAEK graft was clear and well-centred. Uncorrected visual acuity was 20/200. The patient was determined to have recurrent erosions and visual decline attributable to EBMD. Epithelial debridement was performed and the epithelial defect healed by day four. BSCVA at last follow-up four months post-debridement was 20/30-2 with a plano refraction. Trace epithelial irregularity was noted and symptoms of recurrent corneal erosions had resolved.
In case 2, a 58-year-old male complaining of fluctuating vision in both eyes, worse in the left eye, was diagnosed with Fuchs endothelial dystrophy. BSCVA was 20/25 in the right eye and 20/50-2 in the left eye. On slit-lamp examination, confluent guttae were noted in both eyes. The left eye also had central stromal and epithelial oedema. Visually significant cataract was noted in the left eye. Pachymetry was 598μm in the right eye and 705μm in the left eye. Keratometry mires were 4+ distorted in the left eye. The patient underwent staged surgeries in the left eye with phaco/IOL followed one month later by DSAEK. BSCVA was 20/40 by one month post-DSAEK. One year after DSAEK, the donor lenticule remained clear and well-centred. However, BSCVA declined to 20/60-2 and epithelial cystic changes were noted in the entrance pupil. Hard contact lens over-refraction yielded a visual acuity of 20/50-1. It was determined that the epithelial changes were contributing to decreased vision and epithelial debridement was performed. By two weeks post-debridement, BSCVA improved to 20/30-2. At last follow-up, eight months after debridement, BSCVA was 20/25-2 with a smooth epithelial surface.
Summary
EBM abnormalities and endothelial dysfunction are both common findings in the general population. EBMD is an important but often overlooked cause of decreased visual acuity, especially in the setting of endothelial disease. When recognised and treated, it may prevent or delay the need for more invasive surgery or assist in more reliable keratometric measurements so that a favourable surgical outcome can be achieved. Epithelial debridement for EMB abnormalities offers a relatively non-invasive and easy method of normalising the surface epithelium and reducing visual morbidity in the setting of endothelial disease.